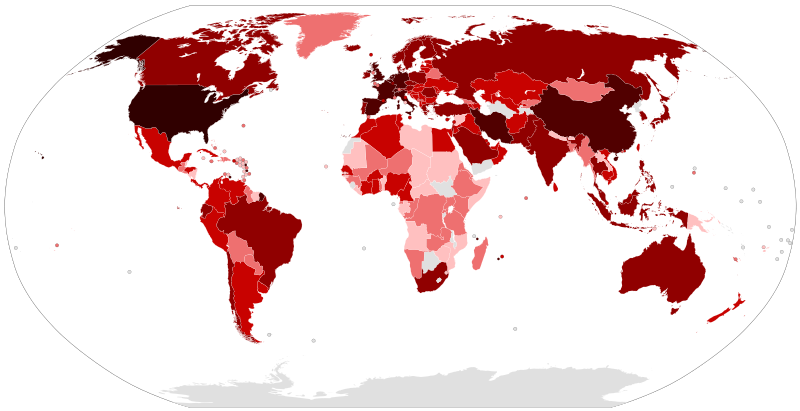
Triage and resource allocation during crisis medical surge conditions (pandemics and mass casualty situations)
A position statement of the Christian Medical and Dental Associations
DOI:
https://doi.org/10.15566/cjgh.v7i1.387Keywords:
triage, resource allocation, resource reallocation, pandemic, epidemic, mass casualty incident, ethics, stewarshipAbstract
The Christian Medical and Dental Associations (CMDA) was founded in 1931 and is made up of the Christian Medical Association (CMA) and the Christian Dental Association (CDA). CMDA has a current membership of over 19,000 physicians, dentists, and other allied health professionals. During and in direct response to the pressing urgencies of the COVID-19 universal pandemic of 2020 the President of CMDA commissioned a special task force to provide current and future Christian reflection and guidance on triage and resource allocation policies during pandemics and other forms of crisis surge medical conditions (e.g., mass casualty situations). This is a condensed version of the CMDA special task force position statement.
References
Ryus J and Baruch J. The duty of mind: ethical capacity in time of crisis. Disaster Medicine and Public Health Preparedness. 2018; 12: 657-662. https://doi.org/10.1017/dmp.2017.120.
University of Pittsburgh School of Medicine, Department of Critical Care Medicine. Allocation of scarce critical care resources during a public health emergency; 2020. Available from: https://ccm.pitt.edu/sites/default/files/UnivPittsburgh_ModelHospitalResourcePolicy.pdf.
Beauchamp TL and Childress JF. Principles of biomedical ethics. Eighth edition. New York: Oxford University Press; 2019.
Edelstein L. The Hippocratic Oath: text, translation and interpretation. Baltimore: The Johns Hopkins Press; 1943.
Kilner, J. Who lives? Who dies? Ethical criteria in patient selection. New Haven: Yale University Press; 1990.
Institute of Medicine Committee on Guidance for Establishing Crisis Standards of Care for Use in Disaster Situations. Crisis standards of care: a systems framework for catastrophic disaster response. Washington, DC: National Academies Press; 2012. Available from: https://www.ncbi.nlm.nih.gov/books/NBK201063/. https://doi.org/10.17226/13351.
Callahan D. Setting limits: medical goals in an aging society. New York: Simon and Schuster; 1987.
Scripture quotations marked (NIV) are taken from the Holy Bible, New International Version®, NIV®. Copyright © 1973, 1978, 1984, 2011 by Biblica, Inc.™ Used by permission of Zondervan. All rights reserved worldwide. www.zondervan.com The “NIV” and “New International Version” are trademarks registered in the United States Patent and Trademark Office by Biblica, Inc.™.
Rubinson L, Hick JL, Hanfling DG, Devereaux, AV, Dichter, JR, Christian, MD, Talmor D, Medina J, Curtis, JR, and Geiling JA. Definitive care for the critically ill during a disaster: a framework for allocation of scarce resources in mass critical care. Chest. 2008; 133(5 Suppl 1): 51S-66S. https://doi.org/10.1378/chest.07-2693.
Texas advance directives act. Texas Health and Safety Code. 2020; §166.046.
Chang A and Walter LC. Recognizing dementia as a terminal illness in nursing home residents. Archives of Internal Medicine. 2010; 170(13): 1107-9. https://doi.org/10.1001/archinternmed.2010.166.https://doi.org/10.1056/NEJMra031087
Downloads
Published
How to Cite
Issue
Section
License
Christian Journal for Global Health applies the Creative Commons Attribution License to all articles that we publish. Under this license, authors retain ownership of copyright for their articles or they can transfer copyright to their institution, but authors allow anyone without permission to copy, distribute, transmit, and/or adapt articles, even for commercial purposes so long as the original authors and Christian Journal for Global Health are appropriately cited.
This work is licensed under a Creative Commons Attribution 4.0 International License.






40.jpg)

.jpg)
1.jpg)