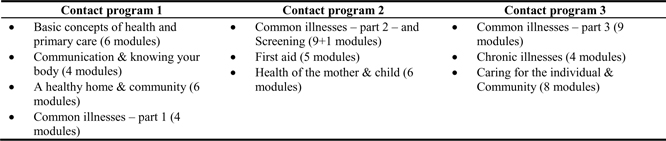
Figure 1. CLHTC Contact Program Outline
ORIGINAL ARTICLE
Nicole Butchera, Adeline Sittherb, Jachin Velavanc, Elizabeth Johnd, Mary Chandra Thomase, Nathan Grillsf
a BSc. MIPH, Research Assistant, The Nossal Institute for Global Health, Australia
b MBBS, CLHTC Course Coordinator, Distance Education Department, Christian Medical College, Vellore, India
c MBBS, DNB (Family Medicine), MRCGP(Int), PGDDE, Coordinator, Department of Distance Education, Christian Medical College, Vellore, India
d M.Sc (Nsg), Masters in Dist Edu (MADE), Senior Nurse Educator, Distance Education Department, Christian Medical College, Vellore, India
e MBBS, MPH, External Faculty, Distance Education Department, Christian Medical College, Vellore, India
f Public Health Physician (FAFPHM), Senior Researcher, The Nossal Institute for Global Health, Australia
Community health workers (CHWs) have long played a key role in delivering healthcare in rural and remote populations, through primary care, prevention, and education. Numerous mechanisms of training and supporting CHWs have been implemented, and the World Health Organization (WHO) has outlined recommendations for the programmatic and financial aspects of CHW programs. This study evaluated the outcomes of a CHW training program in India whereby community development workers from faith-based organisations have been trained since 2011 to extend health promotion, education, and basic services to rural, remote, and poor communities across the country. Triangulation of quantitative and qualitative data and course information was conducted, and analysis pointed to the effectiveness of the trainees in their respective work locations. Outcomes were noted in these areas: health promotion (trainees had gained skills and confidence to implement health promotion interventions); first aid and primary care (graduates were treating common conditions in the community); beneficiary diversity (rural and poor beneficiaries were frequently cited as well as trainees and their families); and, spiritual health (the nurture of person was an important part of conducting CHW activities). The consistency of the data across these areas suggests that the training course is effective in its delivery, its contribution to the expansion of healthcare coverage, and its potential for impact across India.
From Alma-Ata1 to the present universal health coverage paradigm,2 community health workers (CHWs) have consistently played a key role in pursuing “health for all,” particularly for rural and disadvantaged communities. Known in various contexts by a host of names — community health volunteer, lay leader, physician assistant, multipurpose health worker, or other — CHWs are typically members of their community who provide a “reasonable level of healthcare to underserved populations.”3
Models of training, supervision, and development of CHWs have varied over time and differ between contexts. Irrespective of the context, the quality of training largely determines the quality and effectiveness of the particular CHW program. As such, multiple models of training have been developed to promote effective CHWs and programs.3-6
India has a poor record of ensuring access to affordable services for poor and geographically isolated populations.7 With a population of 1.34 billion,8 and 67% living in rural areas,9 a model of disseminated CHWs is essential to provide accessible healthcare. Realising this, in 2008, the National Health Mission of India capitalised on the existing CHW model in conceiving of and implementing the Accredited Social Health Activists (ASHA) program.7 These government-supported community health workers have helped make progress towards improving health coverage in India, though non-government health and development workers help bolster the government systems, particularly in rural and remote areas.
From 2011 to 2014, the Christian Medical College of Vellore conducted a needs assessment among 770 community lay leaders in rural and remote locations across India and analysed 100 of them by regional randomisation. It assessed health indicators in the lay leaders’ workplaces, including proximity of health facilities, availability of doctors, health-seeking behaviours in the community, accessibility of maternal health services, maternal mortality, vaccination, and payment mechanisms. The results quickly established grounds for training respondent candidates to become community health workers, to address the poor health indicators, and thus, the community lay leaders health training certificate (CLHTC) course was designed and launched in 2011.
Taking an intentionally holistic approach to health and wellbeing —, i.e., addressing the spiritual, emotional, and social, as well as the physical — the course seeks to enhance efforts to respond to the high burden of largely preventable and often easily treatable disease. Trainees are church leaders, staff of non-government/faith-based organisations (NGO/FBO), and other volunteers serving rural and underserved areas. They receive the necessary knowledge, skills, and attitudes to serve additionally as basic community health workers. Eligibility criteria for trainees are as follows: (1) twelfth standard equivalent education level or completion of a two-year theological degree, (2) commitment to serve people in the remote areas, and (3) residence in remote areas where access to and quality of medical facilities are poor. Master Trainers are CMC nursing staff. Regional Trainers are mission hospital nurses.
Now in its fifth year of operation, the course trains over two hundred lay leaders each year, equipping each of them to serve around ten villages and three village schools. Their role is to provide basic health care to villages, to conduct school health programs, and to share their knowledge and skills with those in the villages.
This study aims to evaluate the early effectiveness of the CLHTC training program in equipping “lay leaders” to serve — in addition to their ongoing work — as CHWs in India inherently supplement the work of existing/other CHWs. The study assesses the ways in which course graduates contribute to a sustainable and trained community health workforce serving rural and poor communities.
An evaluation of the CLHTC course was conducted by means of triangulating (1) a quantitative survey of 269 graduates from the 2014 and 2015 cohorts, (2) course data on numbers completing the course, and (3) qualitative questioning on the course effectiveness. There was a 78% survey response rate amongst the 344 trainees who attended the graduation/refresher training, representing 38% of all trainees who have so far completed the course.
The survey of course graduates was carried out at the graduation and refresher events at CMC Vellore in South India and at Kacchwa Hospital in North India. Trainers at CMC Vellore designed the survey; the questionnaire had 29 questions and was issued to participants present at the refresher training. Each question was projected on a PowerPoint slide and explained by the CMC Vellore facilitator. Participants responded in handwriting on individual paper response forms.
Thematic analysis, corroborated by two researchers, was undertaken on the qualitative data to arrive at themes regarding the impact of the course on trainees and their communities. Simple descriptive analysis was undertaken on the quantitative survey data to supplement the qualitative data.
Ethics approval was not required under the common rule, as this was an evaluation of an existing program and de-identified survey data was being gathered.
Completion of the course entailed attendance three times at one of 23 training sites for 22 days and studying ten lessons that contained several modules each (Figure 1). Between contact pro-grams, participants had course work to complete in their normal work setting.
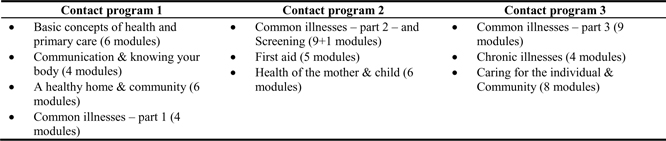
Figure 1. CLHTC Contact Program Outline
A total of 708 candidates have completed the course across 23 training centres (Table 1).
| Year of completion | Graduates | Training centres |
|---|---|---|
| 2012 | 112 | 10 centres |
| 2013 | 178 | 15 centres |
| 2014 | 163 | 19 centres |
| 2015 | 255 | 23 centres |
| Total | 708 | 23 centres |
The graduates surveyed were working in 27 states and territories around India, plus Nepal (1 respondent) and Myanmar (2) (Figure 2). The working locations of five respondents were unknown (“unk”).
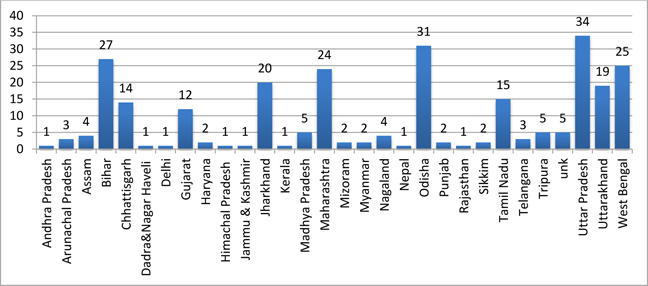
Figure 2. Geographic distribution of respondents
Every two years, a refresher course is conducted over two days at CMC Vellore and Kacchwa Hospital. Attendance is optional and on-site expenses are covered (food, accommodation). The CMC Vellore CLHTC records show that around three in four graduates have attended the two events since inauguration.
The survey respondents work across 27 states in India, except the two working in Myanmar and one in Nepal. They had an average age of 35 years, ranging between 18 and 58 years. Two-thirds (65%) were male, two-thirds (65%) were full-time ministry workers, and the remainder were of various professions and occupations, including among others teaching or working with children. Less than 10% (n=20) had received prior health or medical training.
Thematic analysis of the qualitative responses concerning how completion of the course had affected the ability of trainees to conduct health assessments or provide health care and connect with their community revealed four main outcome categories. The quantitative data supported the themes and sub-themes presented below (with the exception of spiritual health) and have been integrated into the following presentation of the thematic data analysis.
1. Trainees gain skills and confidence to provide health promotion interventions
First, the interviews and surveys revealed that trainees had been equipped to undertake prevention and health promotion and, by extension, raise awareness and prevent diseases. Nearly all (96%) of the respondents said that after the training they “understood the importance of health communication and the ways to communicate health messages.” Over half the respondents (58%) reported “doing preventive work” more than once per month, and one-quarter on a once-monthly basis. Particular areas where prevention and promotion activities were reported as being undertaken were women’s health and NCDs.
Concerning health education in the villages where they served, respondents S163 and N13 said,
Recently I was able to teach 200-250 women and girls about the care of pregnancy, puberty care, marriage, self-examination. Everyone got use of it even experienced women who came from Hyderabad. (S163)
After this course I explained to the people in my village the various ways in which diseases spread and how we can prevent them … [W]e used to get a lot of diseases in the village. Now we have understood the reasons for the same and are able to prevent them. (N13)
The trainees also reported being involved in various screening programs and, thus, promoting early detection, referral, and treatment of diseases such as diabetes. This was evident in individual cases, in workplaces, and community groups:
We found a pregnant woman to be anaemic while visiting a village. We gave her health education about pregnancy. She delivered the baby safely. (S2)
As we are doing children ministry, now I can do screening for all the children who are coming for the children’s camp. Now we can teach to our [children] whatever I learnt in this training. (S165)
Since Malto people live in the hills, they don’t get medical help easily because of the hospital distance. Once when checked, more than 70% of the people were affected with anaemia. I gave health education on diet — green leaves, vegetables, nuts, and peas. After two months, when we checked again, there was a good improvement in them. (S-unk-1)
2. Teaching diagnostic skills enables CHWs to provide needed treatment
Second, the course has equipped the trainees to respond to a variety of illnesses through first aid, making clinical diagnoses of and managing certain common simple illnesses, and making appropriate referrals. Nearly all (97%) of trainees reported being either confident or very confident to be able to carry out healthcare tasks such as checking blood pressure and administering first aid. Respondents N47, S118 and N12 commented:
I help more people by these tools. One time, someone got bitten by a snake. Then I took him to [the] doctors and saved his life. (N47)
A boy met with an accident and was bleeding profusely. I placed his leg in a higher position and pressed it, thereby preventing more loss of blood. (S118)
This training has been very useful in my ministry. Diabetes is a disease very prevalent in my place of work. Out of ten people that I checked, three people were suspected to have diabetes, and I referred them to Herbertpur hospital. Now they are undergoing treatment for the same. (N12)
In line with trainees’ responses to illness and disease, tuberculosis and diarrhoea were raised repeatedly in stories of trainees having intervened and made a difference in their communities. Respondent N2 reports about a student who got infected with TB, saying, “He became so discouraged to even tell his parents. I helped him get DOTS treatment fully. Now [he’s] fully healed.” By educating his community about diarrhoea, respondent S12 saw pleasing results in one family’s life:
I taught about diarrhoea. How to prevent and make ORS. Our believers are using ORS so now they [are] alert. [For] two years one child had diarrhoea. [For] two days he could not able to walk. His mother prepared ORS and gave [it to him]. Then he got up and started to play.
Respondent N67 has been able to make a dramatic difference in the life of one woman who had been suffering from diarrhoea several times monthly for the past seven to eight years. He/she taught her household about water safety:
I went to their house to find out the issue and realised that they used to drink water from a vessel in which they dipped their tumblers with dirty hands to take water. I taught them that it is wrong. From then, the woman has stopped having diarrhoea. (N67)
Most respondents (89%) reported strong agreement with the statement, “The training on practical skills and other sessions were beneficial for our actual role in the field,” and many were enthused by the outcomes they experienced personally through application of their new knowledge and skills. Respondent S95 testified:
It is very helpful to me. Once I recognised a patient who had rheumatic fever. When he went to the doctor, the doctor declared he is a patient of rheumatic fever. Then doctor started treatment and slowly that person got well. It was very exciting to me. (S95)
Concerning medication, around two-thirds (69%) of respondents give medicines “sometimes,” and equal parts of the remaining third do so never or often. A number of the participants added comments about giving medicines to those in their villages (according to the instructed protocols).
3. CLHTC reaches a diversity of beneficiaries, in particular the rural and poor
Third, respondents reported how CLHTC was benefiting their own families, churches and communities, and, in particular, populations in rural and disadvantaged areas. Two-thirds (69%) of respondents apply their knowledge and skills in an opportunistic manner, one-third (33%) in their church, and around half (53%) at organised health promotion events.
A focus on helping the poor and marginalised was evident through the qualitative responses:
I live in a very poor area so this training is very helpful for me and my community. I used [it] for awareness programs. (S28)
Treated and prayed for Kalpna who was ill and belonged to a poor family. (S3)
Abundantly helped in my ministries. Especially our rural and semi-rural areas where [there is] no medical opportunity. (S42)
… [I] help the people working in a remote area. It [CLHTC] helps me to teach them about clean environment, making toilet for the people. (S59)
We stay in a remote area with many tribals… In my field, many are TB and pneumonia patients. We visit them and find symptoms and take them to medical (services). Also we find skin problems. We advise them and give some medicine. (S75)
Most (97%) respondents said that they are either confident or very confident to teach village health volunteers in their area. Several trainees explained how they are playing an active role in knowledge and skills multiplication and using a community development approach:
Taught health education with practical lessons (e.g., ORS) to our home (hostel) children and they in turn teach their families. (N2)
In the place where we work there were a lot of deaths. We sat together with the community and came to the conclusion that it was due to the drinking of liquor. We taught the villagers the ill effects of drinking [alcohol] and now slowly people are giving up the habit and are happy. (N7)
4. Spiritual health is an important component of healthcare
Finally, most respondents mentioned the importance of the spiritual aspect of the health work they carried out. In part, this relates to improved relationships: 88% of graduates have gained increased acceptance in their workplaces:
CLHTC helped me build relationships with my family, village and society and thereby en-couraged people and took the church forward. It help me to communicate with people easily. (S70)
There were families in the village who would not listen or invite us but now they are inviting and listening and learning. (N9)
It also refers to the avenue graduates have gained to minister to people’s spiritual needs as part of treating their physical condition:
I am the pastor of a church. Whenever I visit believers, if they have any headache, viral fever, [or] body pain, I give them some medicines and pray to God for their healing. Not only among the believers, but also with non-believers I do give and have been praying for them. (N36)
In addition, the trained workers help counter mysticism and medical illiteracy through educating villagers:
Before I joined the course I used to only teach from the Bible. I didn’t have any information about the diseases and used to say that it’s from the devil, pray for the disease and send the patient away. But now after I’ve done the training I can examine the patient and teach him/her about the disease and treat whatever is possible. (N11)
Respondents were virtually unanimous in their testament to the effectiveness of the course, affirming that CLHTC benefited their knowledge, skills, and confidence levels. It had moreover caused the strengthening of relationships between graduates and their communities, an observation that corroborates WHO’s statement that CHWs “can go beyond the provision of care and foster community-based action.”2
The results also showed evidence of improveing graduates’ own health and that of their families. Although trainees were not the intended direct beneficiaries, it is appropriate and advantageous for families working in rural and remote areas with little access to healthcare. That is, they need to be able to maintain their health, self-diagnose, and know when to seek further medical attention. This course might contribute incidentally, therefore, to the longevity of these workers staying in rural areas.
It is noted that CMC Vellore does not deliver this course in order to establish a CHW program, per se, but to produce health worker graduates for remote locations across India. As such, this isolated investment in CHWs may not optimise synergies of CHW programs across India as per the WHO’s recommendations,2 and some of the operational elements of a CHW program are lacking,5 e.g., individual performance evaluation, and information management. However, the “hub and spokes” model of the course — whereby CMC links CLHTC graduates to the local hospital/training site — allows for a certain degree of support and monitoring. Also, course graduates have reported in both quantitative and qualitative responses that they make referrals to medical services, through which the treating practitioners can partially gauge the quality of first-aid treatment and response.
With respect to information management and monitoring of outcomes, it would be valuable to repeat the study that was conducted as a needs analysis to observe changes to indicators that were reported when training was established. Some indicators of referrals and drug administration (and other, including spiritual) could be incorporated to provide additional insight into the impact of graduates serving as CHWs. For example, a validated and standardised survey could be completed by the trainees (or a representative sample) at enrolment (time=1), at completion of the course (time=2), and at a specified period after completion of the course (time =3). Indeed, as the number of trainees increases and the course expands, there is a growing need for systematised and comparable data collection from the trainers, trainees, and field sites. This is necessary to facilitate improvements to the course as well as gather quantitative measures of the impact of the course on health indicators.
Concerning the training curriculum, WHO stresses the importance of developing trainee competencies, such that the trainee graduates with experience in a blend of promotive, preventive, therapeutic, and rehabilitative services.4 The data gathered here suggest that the CLHTC course has achieved this mix in the training and has effectively equipped workers with promotive, preventive, and therapeutic community health skills. It should be considered if this training might be relevant for other similar low- and middle-income settings. To this end, the trainees from Myanmar and Nepal have already successfully completed the course. However, as recommended by the WHO,4 training would need to emphasise applicability of the knowledge and its relevance to the social context of the learner.
Concerning the trainees proper, two-thirds of the survey respondents were male, whereas in other CHW training courses in India, and indeed internationally, female trainees are typically greater in number. ASHA workers, for example, are exclusively females. These gender-based findings reflect the minimum education requirement for entry to the course, but may also reflect the fact that many full-time ministry workers based in rural India are men. As it happens, training males who are working in rural, poor, and hard-to-reach areas may be an appropriate strategy for reaching those very beneficiaries.
Finally, noting that 72% of respondents came from faith-related occupations, it is not surprising that the qualitative results had a strongly spiritual focus. Nevertheless, it suggests that the training equipped them to think and function with a holistic or integral approach, which is also contextually appropriate insofar as the Indian patient commonly expects to receive both the medicine (dawa) and the blessing (duwa) from an encounter with a health practitioner.
Both the qualitative and quantitative questions in this survey asked the trainee to self-report the change in their knowledge and practices. As such, the results do not provide an objective understanding of graduates’ proficiency of knowledge or skills before or after the course. Also social desirability bias is a relevant concern given the strong relationships with the training institution, as indicated in the qualitative data. However, the survey forms were designed for anonymous and individual completion in order to minimise pressure on respondents from peers and/or staff to give a positive response.
Similarly, the survey did not ascertain the level of trainees’ exposure to health-related incidences or assistance in health-related matters (prevention, education, referral, etc.) prior to the course. Ideally, a baseline would have been undertaken to gain an understanding of trainees’ prior health knowledge and practices. However, it is assumed that such health-related knowledge and actions were minimal given that most trainees reported having no prior health or medical training.
Again, the quality of healthcare provided by the graduates cannot be determined from this study. However, these candidates have passed three sets of formal exams set by CMC Vellore that has ranked as India’s second leading medical college for maintaining high standards in teaching, assessment, and certification of graduates.10
Finally, the sample only included those who graduated and attended refresher training sessions. This may have created some selection bias towards enthusiastic and well-performing trainees. However, this would be limited, given that the sample represented over one-third (38%) of those who had ever completed the course.
A large workforce is needed to meet India’s health needs. As trained health personnel are unwilling to move to the villages of India, the CLHTC health worker training course demonstrates potential to train thousands of community health workers to work in disadvantaged rural/remote areas. This well-designed training program conducted by a premier institute, focused on knowledge, skills, and attitudes, using already-established regional centres based in rural India, and employing nurses based in these centres as trainers, is drawing out NGO/FBO workers to make a significant contribution to the health and wellbeing (including the spiritual health) of particularly disadvantaged populations. These trainees who already live among the poor and are committed to their wellbeing are increasing the accessibility of healthcare services and, thus, hold the potential to substantially reduce incidences of illness and disease.