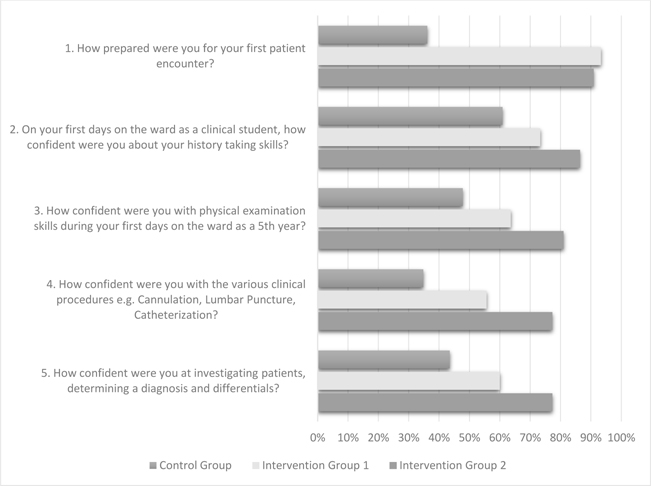
Figure 1. Impact on pre-clinical skills training and the addition of PAL on preparedness and confidence in medical students.
ORIGINAL ARTICLE
Cheryl Snydera, Rose Chisengab
a MA, DO, Associate Professor and Chair of the Science Department, San Diego Christian College, United States
b MB ChB, Junior Resident Medical Officer, University of Zambia, Zambia
Background: Many benefits of pre-clinical medical skills training have been documented in technologically advanced nations, and in the past decade these courses have been introduced to developing countries. Curriculum that can prepare and build confidence in medical students must be cost effective, evidence-based, and culturally sensitive in places where there are severe resource limitations. In 2013, an initial pre-clinical skills course without assessments was introduced to medical students in Zambia. Later that year, a more developed course was launched to a second cohort integrating Peer Assisted Learning (PAL) and assessments. These trainers were prepared in advance with instructions in standardized skills, learning theory, effective feedback techniques, and use of rubrics to insure good inter-rater reliability in teaching and assessments.
Methods: A quantitative study surveyed 108 students utilizing convenience sampling and a written questionnaire. Data collected compared preparedness and confidence in performing clinical skills of the intervention cohorts with the control group (medical students who preceded pre-clinical skills training).
Results: Preparedness responses increased from 36.1% of the students in the control group to 90.9% in the intervention group who had been exposed to the PAL course with assessments (p value <0.001). Student confidence levels in history taking, physical exam skills, procedures, and the application of critical thinking skills diagnostically also showed improvement from 11.5-29.5% range in the control group to 77.3-86.4% range in the PAL cohort (p value <0.001).
Conclusions: Exposure to pre-clinical training program especially utilizing PAL with assessments had a positive impact on the sense of preparedness and confidence levels for medical students beginning their clinical training years at the University of Zambia. Integration of PAL influenced academic development, clinical procedural standardization, appropriate curriculum additions, transitional support, and program sustainability. PAL may have beneficial application extending to basic science lab instruction in resource limited environments. Recommendation for future research would be integration of qualitative triangulation and reduction of variables in confidence data reporting.
The benefits of pre-clinical skills training during the medical school years are well researched in technologically advanced nations and include the following: reduced workload for clinical faculty, decreased anxiety for the student, and improved patient safety.1-5 Curriculum that is cost effective, evidence-based, and culturally sensitive is a critical consideration throughout the world but even more so in developing countries where there are severe human and financial resource limitations.6-8 By 2012, pre-clinical medical skills training had been introduced into other African nations, however a literature search failed to report on cost-effective curriculum or evidence-based methodology.
Sub-Sahara Africa in general and Zambia specifically have experienced high rates of poverty and health challenges. The Human Immuno-deficiency Virus (HIV) is listed as the most common cause of death (20%) according to the Center for Disease Control (CDC) statistics for this nation.9 The Ministry of Health (MOH) addressing the Deans of Zambian medical schools in 2012 estimated the country to have a physician shortage of at least 2000 and encouraged increased medical school enrollment. In response, the University of Zambia, School of Medicine (UNZA SOM) expanded the medical class size from 60 students per year (class of 2014) to approximately 170 students per year (class of 2019). The tasks of training, supervising, and assessing students’ clinical skills became even more onerous for the already over-worked clinical faculty. In addition, the students typically lacked any formalized pre-clinical skills training when they began their clinical years working with the “sickest of the sick” at a tertiary referral center, the University Teaching Hospital (UTH) in Lusaka.
UNZA SOM has a seven-year medical school curriculum, and students are introduced to their first clinical experience with patients at the beginning of their fifth year of medical school. Prior to September 2013, students were oriented to the expected skills by whoever was available for that specialty (consultants, residents, interns, fellow students, etc.). At most clinical rotation sites, students reported their orientation experience to be “unstructured” and “inconsistent.” Clinical rounds took place with up to 30 students gathered around a patient’s bedside to observe a physical exam. Physician supervision of individual students performing exams and procedures was rare. Objective Standardized Clinical Exams (OSCEs) were just being introduced on some of the clinical specialty rotations for assessment of skills. Patient exams occurred primarily in a discussion format (patient remaining in a chair) and physicians demonstrated limited physical exam and diagnostic skills. In addition to insufficient supplies and patient delays in seeking medical care, mortality rates were high with the average life expectancy in 2010 estimated at only 58 years compared to 78 years in the USA.10
In an attempt to rectify some of these concerns at UNZA SOM, a new curriculum component was introduced in January-March 2013 as a pre-clinical skills course (32 contact hours). The ratio was one experienced physician to train 96 fourth-year medical students (Group 1). Two-hour didactic classes introduced the basics of history taking, physical exam, differential diagnosis development, and procedures (intravenous and Foley catheterization, nasogastric tube placement, and lumbar puncture), and a summative didactic exam was given. Lab sessions lasted 2-4 hours per week where students practiced skills on simple, non-electronic manikins and classmates. However, due to the lack of examiners, skills assessments did not occur. Students, consequently, still reported a lack of confidence as they prepared to enter their clinical years.
In an effort to improve the curriculum and bolster confidence in UNZA SOM students transitioning from the pre-clinical to clinical training levels, Peer Assisted Learning (PAL) was introduced. This methodology involved the recruitment and training of sixteen volunteers, more senior (5th-, 6th-, and 7th- year) medical students who were provided an 80-hour program. Concepts of learning theory, inter-rater reliability, mentorship, and providing quality feedback were introduced. Trainees were expected to demonstrate standardized clinical skills (procedural and physical exams) in both the student and teacher roles. Feedback and evaluations in a 360-degree manner (supervising physician, peers, and the trainee themselves) were given throughout the program to help develop the expected supportive culture for this new role. These peer educators were required to assist with the development of procedural rubrics and writing of culturally appropriate standardized patient histories. After a mock psychomotor assessment, the training group compared rubric scores in a discussion format. Trainers learned to identify if they were either too strict or too lenient in their assessment skills (and modify when necessary).
Subsequently, a second pre-clinical skills course was offered to the second cohort of 36 fourth-year students (Group 2). The course was slightly longer than the first, spread over eight weeks (50 student contact hours). There were combined classroom didactic lectures in the mornings given by the training physician and senior peer educators with supervised practice lab sessions required in the afternoons. Students were expected to practice physical exam skills with one another during the evenings and weekends. In addition to the initial skills of intravenous and Foley bladder catheterization, lumbar puncture, and nasogastric tube placement, more advanced skills were introduced including airway management, cardiopulmonary resuscitation, and one standardized patient encounter.
Research on the impact of the pre-clinical course on student preparedness and confidence levels as well as the specific impact of PAL with assessments on the second cohort is described below. After the initial two shorter courses, a full year course was launched in August 2013-May 2014 and a second year-long course the subsequent year.
The research design utilized a convenience sampling, quantitative approach comparing the intervention groups (1 and 2) with a control group that had not received skills training. The study focused on student perception of preparedness and confidence levels. Ethical approval as an exempt research project was granted by UNZA Biomedical Research Ethics Committee (UNZA BREC) and also by the Institutional Review Board at the University of New England, USA. Data was collected from a printed questionnaire that took students approximately five minutes to complete. An explanation of the purpose of the survey and ethical considerations of this volunteer-dependent research was provided verbally. The participants were informed that the results would be treated confidentially and used for curriculum development (i.e., specifically not impacting grades, advance-ment, or employment).
The research questionnaire had two portions, demographics and the research questions. The basic demographic information included date, current year of study (5th, 6th or 7th), gender, the specific rotation that occurred as the first clerkship of the 5th year (Internal medicine, Pediatrics, Surgery, or Obstetrics/Gynecology), and timing when the pre-clinical skills course was taken (options were “not taken,” “Jan-March 2013,” or “June-August 2013”).
The five survey questions were as follows:
The response options were in a three-point Likert scale to simplify the process and reduce the time required at the recommendation of the peer trainer involved in question development. The instructions were to circle the appropriate response with three categories of choices as potential answers:
The setting of the survey was at the University Teaching Hospital (UTH) in Lusaka, Zambia, a tertiary facility and the primary clinical teaching site for 5th, 6th, and 7th year UNZA SOM medical students. The convenience sampling of the students (intervention and control group) was based on the availability of the participants at UTH during one specific week (October 2013) and their willingness to participate in taking the anonymous survey given by preselected academic assistants. The targeted sample sizes for the control and intervention groups were 33% of the potential pool of respective participants. Typically, due to responsibilities of these students in patient care areas or being at home post call, less than 50% would actually be available during random time blocks at the UTH site. Demographics of the prospective pool placed them primarily in the 20-30-year-old range, mixed gender with ratios of approximately two male students to one female student, 95% of African ethnicity, and 5% a mix between East Indian and Middle Eastern ethnicities.
The survey was anonymous and had no personal identifying information beyond demo-graphics mentioned above. Peer educators were excluded from the survey due to potential bias. After collecting the completed questionnaires, the surveys were divided as follows based on student’s exposure to pre-clinical skills training:
Control group: The control group included 61 participants (potential pool of 139), 6th and 7th year students, without any exposure to the pre-clinical skills course.
Group 1: This was an intervention cohort of 23 participants (potential pool of 96), 5th-year students exposed during their 4th year to the initial pre-clinical skills course during January-March 2013. Skills included physical exam, intravenous and Foley bladder catheterization, nasogastric tube placement, and lumbar puncture). No assessments were required.
Group 2: Another intervention cohort included 22 participants (potential pool of 36), fifth-year students, exposed to the second pre-clinical skills course during June-August 2013. Skills included those listed above as well as airway management, cardiopulmonary resuscitation, and one standardized patient encounter. This cohort also had PAL, and clinical skills assessments were required during a summative exam.
A total of 108 questionnaires were completed and returned, two were excluded based on criteria (5th year students who had not attended the course). Sixty-one (43% of the potential pool) of the returned surveys were from the control group (6th- and 7th-year students who had not experienced pre-clinical training) and forty-five (34% of the potential pool) were from the intervention groups (combined).
Data were grouped from the three-point subjective Likert scale into a binary model to better view change versus no change. “Prepared” and “very prepared” responses were summed and compared with the “not prepared” responses. Likewise, the number of “very confident” and “confident” responses were summed together and compared to the “not confident” responses. Question 3 was not answered by one student in group 2; this was noted but the rest of the survey responses were complete.
Statistical analysis was conducted using Epi Info version 3.5.4 stat calculator utilizing Chi-squared test (Mantel-Haenszel method) on the tabulated data.
The pre-clinical skills course positively influenced the students’ sense of preparedness and confidence levels with the most dramatic changes in confidence seen in the second cohort exposed to PAL methodology with assessments. Question 1 indicated only 36.1% of the students in the control group acknowledged a sense of preparedness for their first patient encounter, compared with 90.9% reported by the intervention group exposed to the PAL course (p value <0.001 Table 1).
Student confidence levels in performing the various benchmarks of history taking, physical exam skills, procedures, and the application of critical thinking skills diagnostically also showed positive improvement after the introduction of the course. The control group reported 11.5-29.5% range in confidence in those skills compared to 77.3-86.4% range in the intervention group 2 after PAL methodology was introduced with assessments (p value <0.001 Questions 2-5 Table 1).
The data indicates that the initial student cohorts exposed to the course were more confident than those who had no course. However, the second cohorts who participated in the PAL methodology with assessments during the pre-clinical skills course were the most confident in their skills starting out in their clinical rotation (Figure 1).
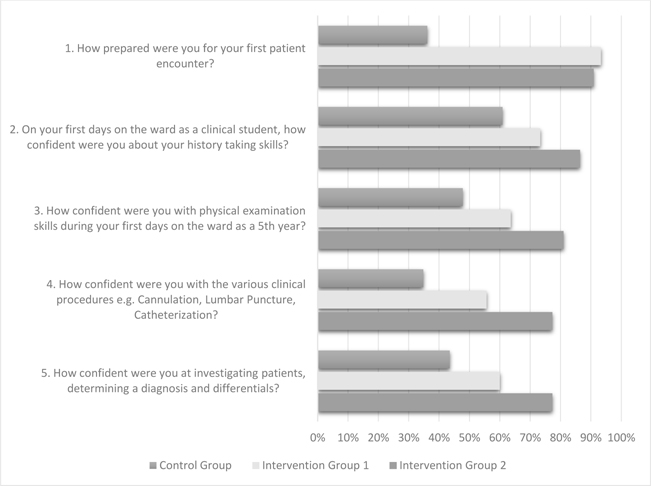
Figure 1. Impact on pre-clinical skills training and the addition of PAL on preparedness and confidence in medical students.
The short initial pre-clinical skills course was effective in generating a sense of preparedness in the Zambian medical students consistent with the findings by researchers in developed countries.11-16 Falk et al. specifically documented improved confidence in clinical skills of students preparing for surgical internships and though not taught initially, suturing was the skill most appreciated by students as the program developed into a full-year course. Improved student confidence influenced academic progression, clinical procedural standardization, and development of a more culturally sensitive curriculum.13 The medical students found transitional support between the pre-clinical and clinical training areas. Ultimately, those confident students who became peer educators invested their time to sustain the pre-clinical skills program, despite increasing numbers of junior students and decreasing resources.
Peer educator training was initiated prior to teaching the second cohort of junior students and continued weekly throughout the school year. Retention of these trainers was high through the years, and they reported how the program helped them to develop mastery of basic skills. This is consistent with previous research on tutors in other countries.14 An extensive literature review on clinical skills training by Bugaj and Nikendi, published in 2016, referred to Miller’s Learning Pyramid that distinguishes four levels of competence or training objectives - knows, knows how, shows how, and does. As the student transitions from cognitive understanding to competence in performing the psychomotor skills on patients, it is beneficial to not only learn the skill but to demonstrate their abilities. This reinforces the need for practical skills training with assessments.15
Confident peer educators frequently reported a desire to pursue academics after completing their initial medical degree, a difference from their initial intentions. They reported how they enjoyed the “sense of family” that developed amongst the peer trainers as they worked together for the good of their future colleagues. Wenrich et al. specifically researched the impact of a training program on clinical educators over a five-year period of time and noted significant improvement by the faculty in giving feedback to students and understanding their developmental needs. They also reported development of teaching tools and strategies for a more inclusive team approach.16
In time, peer educators assisted with more clinical procedural standardization and culturally appropriate curriculum development. Clinical students who had experienced the pre-clinical skills lab, either as only a student or a student and a peer educator, carried guidelines with them into their clinical years. During the full-year program, residents were also incorporated into the pre-clinical training program and later used these training rubrics for their clinical assessments on more senior students providing consistency between the two areas.
Truly sensitive and culturally appropriate pre-clinical curriculum would not have been possible without the involvement of the developing student educators. Zambia is very culturally diverse with over 72 tribal/cultural groups. By integrating diverse trainers (who represented various tribal groups), a common bridge was established between the pre-clinical program and clinical training sites with appropriate transfer of knowledge. This was essential in the areas of development of standardized patients’ scripts for ‘“Telling Bad News’ and gender-based violence, differential diagnoses, and appropriate patient diagnostic work ups. For example, common presenting illnesses in an emergency department in Zambia were malaria, HIV, and tuberculosis rather than myocardial infarctions, strokes, and obesity-related disorders which are more typically seen in the USA.
The peer educators frequently suggested additional skills needed to better prepare medical students for the clinical experience. For example, when the nurses went on strike, the medical students were responsible for injections but had not received any previous formal training. Neonatal resuscitation was another skill introduced later in the training year after hearing of the shortage of nurse midwives and obstetricians to supervise the increasing number of hospital deliveries. Neonatal resuscitation training utilizing a rubric provided a tool to practice skills safely before they found themselves in a critical life or death clinical scenario.
Transitional support was a byproduct of the PAL methodology and helped students transition from the theoretical academic years into the challenging reality of the clinical experience with more confidence. These stark realities can be dauntingly incongruent as described by previous researchers in resource-limited countries.12 Despite the stress of working without common supplies or sufficient staff in the clinical area, students reported an improved sense of confidence when they saw the familiar face of a more senior peer educator.
Ultimately, through PAL, the pre-clinical training program was sustainable. Typically in a US medical school, pre-clinical skills are provided in small group settings (i.e., one experienced physician to 8-10 students). As previously stated, in Zambia, the program was launched with one experienced physician for 96 students. Utilizing paid, experienced physicians for lab instruction was cost and resource prohibitive, thus the mandatory introduction of the more cost effective PAL methodology.
As they took on the role of peer educators, they were empowered to continue making improvements in the program to better prepare their junior colleagues whether in the pre-clinical lab or at the bedside of the patient. This extension of the impact into the clinical setting has been described in Plack et al’s research studying the impact of a fellowship program at a US institution.17 In Zambia, many additional skills were introduced including multiple standardized patient encounters, triage and disaster response, suturing, skills for pediatric evaluation, pelvic exam, and Objective Standardized Clinical Exam (OSCE) in subsequent years.
As peer-educators’ ownership grew, so did the sustainability of the program. This was evident less than three years after the initial pre-clinical skills course was launched when they successfully trained 40 additional peer educators, followed by 169 fourth-year students during the 2015-2016 school year. This was the largest cohort of students in the medical school’s history and was supervised by national residents independent of expatriate involvement.
PAL is a valuable methodology and could be used beyond pre-clinical skills with proven application in a multitude of other settings where there is a shortage of trainers. Research by Sammaraiee et al. demonstrated this resource application to basic science labs and Shiozawa, et al. specifically showed improved student learning of dissection skills.18,19 Resource limited nations such as Zambia could benefit greatly with PAL methodology in other lab areas to help with sustainability and encourage academic advancement for the trainers.
One limitation of this study includes the paucity of objective testing results that could corroborate the more subjective data. During the time of initiation of this research, 5th-year OSCE scores from the clinical programs were not collated and available. In 2013, some departments still had not launched this type of assessment during the clinical years. However, clinical faculty verbally reported “improvement” when comparing the intervention groups with previous students (without pre-clinical training).
Uncontrolled variables were additional limitations that could have influenced students’ reported preparedness and confidence levels. Considerations include variation in personality, recall bias of the control group, previous curriculum exposure (nursing experience), and actual early clinical encounters and how they correlated with skills taught and attrition of skills. For example, the time between completing the training and beginning the patient encounters for group 1 was 6 months and for group 2 was less than 3 weeks. The use of a three point Likert scale on the questionnaire was time efficient and easy to answer, but limited the accuracy of the range of confidence responses.
Recommendations for future studies assessing the impact of a pre-clinical course include accessibility to correlated clinical OSCE scores, reducing recall bias, increasing qualitative triangulation, and improved specificity in the questionnaire. Self-impression of preparedness and actual readiness based on skills performance can be two entirely different realities and altered with time in the clinical wards. The use of qualitative triangulation has proven beneficial in the research of Plack et al. and suggests that improved preparedness reporting could be obtained through the process of correlating input from clinical faculty, trainers, and the student.17
Exposure to a pre-clinical training program, especially utilizing PAL with assessments, had a positive impact on the sense of preparedness and confidence levels for medical students beginning their clinical training years at the University of Zambia. Integration of PAL influenced academic development, clinical procedural standardization, appropriate curriculum additions, transitional support, and program sustainability. PAL may have beneficial application extending to basic science lab instruction in resource-limited environments. Recommendation for future research would be the integration of qualitative triangulation and reduction of variables in confidence data reporting.