Figure 1: Diagram for sampling and sample size
ORIGINAL ARTICLE
Ghanshyam K Bhattaa, Josue Orellanab, Bidya Mahatb, Ishwar Nath Mishrab, Chandeshwari Tamrakarb, Sujit Kumar Sahb
a Team Leader, Adventist Development and Relief Agency (ADRA), Nepal
b Adventist Development and Relief Agency (ADRA), Nepal
Background: Family Planning (FP) is a key developmental focus for the government of Nepal. Use of modern contraceptives has stagnated at 43.2% since 2011. Unmet need for family planning (FP) in Nepal remains high at 27%. Despite relatively high unmet need, a factor contributing to this levelling of contraceptive use is the limited range of methods available to most clients at most sites. To address the FP need among married women of reproductive age (WRA), we tested integration of FP into agricultural programs.
Aim: To assess the effectiveness of a FP program integrated into an agriculture (e.g., non-health) sector program.
Methods: A descriptive cross-sectional (post interventional) study was conducted November 2015 to February 2016 among 525 WRA participating in an agriculture program.
Results: The contraceptives commonly used by women in the study location were Depo Provera and Minilap. After Technical Integration Coverage and Access (TICA) interventions, almost all of the respondents (99.6%) had heard about FP of which 67.8% correctly understood FP as a method to prevent unwanted pregnancy. About 50% of the respondents were found currently using FP. The percentage of WRA aware of long-acting and permanent FP methods increased from 49.0% to 62.0% and 39.0% to 52.0% respectively. Decisions on using a FP method were predominantly made by the husband (68.0%). However, 68.4% women reported that they were accompanied by their husband. The proportion of men willing to use FP increased from 5.2% to 15.5% after TICA activities implementation. The main reason identified for not currently using FP devices was that the husband and wife were not living together (88.8%). Most of the women (98.0%) reported that FP utilization improved their quality of life.
Conclusion: TICA activities were very successful in both increasing FP knowledge level as well as utilizing FP services among the targeted beneficiaries. The use of FP increased among agriculture program beneficiaries after the integration of TICA activities with a gradual shift from short-acting FP methods to long-acting and permanent FP methods. For easy integration, FP projects should also utilize existing community structures such as cooperatives, women’s groups, men’s groups, and youth clubs.
Key words: family planning, Nepal, development, agriculture sector, contraceptives
Based on global evidence, maternal and child health outcomes could be substantially improved by meeting family planning (FP) needs of women in developing countries. Provision of FP services contributes to a reduction in maternal mortality by lowering the risk of maternal death per birth hence preventing high-risk and high-parity births.1,2 According to the Nepal Demographic and Health Survey (NDHS 2011) and Nepal MDG Progress Report 2010, despite significant progress toward achieving Millennium Development Goal (MDG) 5, “Improve Maternal Health” (decreasing maternal mortality from 539 in 1996 to 229 in 2011), Nepal was unlikely to meet the 2015 MDG 5 modern contraceptive prevalence rate (mCPR) target of 67%. Nepal’s early success in family planning (increasing the mCPR from 2.6% in 1976 to 44% in 2006) had plateaued, and use of modern contraceptives had stagnated at 43.2% since 2011. Unmet need for FP in Nepal remains high: 27% of married women reported unmet need in 2011, up from 25% in 2006. The Government of Nepal’s family planning goal is to achieve replacement level fertility (2.1) by 2020.3,4
Pregnancies at an early age whether planned or not and unwanted pregnancies increase reproductive health risk including exposure to unsafe abortion and maternal mortality. Over half (55.0%) of Nepali women are married by the age of 18 which increases their chance of pregnancy at an early age. Nearly half (47.0%) of girls who had their sexual debut before age 15 are forced against their will. A quarter (25.0%) of WRA in Nepal experience unplanned pregnancies.3
Important disparities in contraceptive use exist. While the overall national mCPR among married women is 50.0%, it is only 19.0% among Muslims, 25.8% among youth (married and unmarried), 37.0% among Hill Dalits, and 41.0% among Hill Janajatis (indigenous). Both Dalit and Janajatis are groups that are traditionally disadvantaged/marginalized. The mCPR of spouses of migrant labourers is also extremely low: 20.0% among women whose husbands live elsewhere for at least one year, with even lower rates in the mountains and the hills (11.0% and 14.0%).3
Among groups with low mCPR, unmet need for contraception is considerably higher than the national average of 27.0%: 39.0% among Muslims, 38.0% among youth, 35.0% among Hill Dalits, and 34.0% among Hill Janajati. Unmet need is also high among migrants, at more than double the national average, and among the poor: 31.0% in the lowest wealth quintile compared to 22.0% in the highest. Unmet need is higher in rural than in urban areas and highest in the Western Hill sub-region (36.0%) and Western region (34.0%). It is similar in Mountain and Terai areas (26.0% in both). Compared to 2006, levels of unmet need in 2011 declined in Mountain and Hill areas but increased in Terai areas.5,6
Another factor contributing to the levelling off of contraceptive use despite relatively high unmet need is the limited range of methods available to most clients at most sites. In addition, poor quality counselling may be hindering clients’ understanding and choice when selecting a contraceptive method. Since 2001, female sterilization has been the most common modern method of contraception in Nepal accounting for 35.3% of all FP users, mostly post-child bearing, followed by male sterilization at 18.1%. 15.0% of married women report using surgical contraception, followed by 9.0% using injectable contraceptives. All other modern methods are at negligible levels, with only 2.8% using implants and 1.3% using Intra-Uterine Contraceptive Devices (IUCDs).3
Limited services in hard-to-reach areas and insufficient community-based FP outreach to hard-to-reach groups has resulted in insufficient contact between FP non-users and FP service providers. Among all women who are not currently using FP methods, only 9.0% were visited by female community health volunteers (FCHVs) who discussed FP, and only 6.0% visited a health facility where they discussed FP. Overall, 88.0% of non-users did not discuss FP with any health worker.3
The Government of Nepal’s FP program aims to have all FP methods (condoms, oral contraceptive pills, injectables, and long acting reversible contraception (LARC)) available at service delivery sites from District Hospitals down to the Health Post (HP) and outreach clinic level. It also aims to have District Hospitals provide voluntary surgical contraception (VSC) services year-round, and mobile services provide comprehensive FP services, including VSC and the full range of temporary methods. Despite this goal of providing district wide comprehensive FP services, poor functioning of institutionalized family planning service centres has been identified as a key issue in FP service delivery. The majority of Health Posts and Primary Health Care/Outreach (PHC/ORC), particularly in hard-to-reach areas, do not provide voluntary LARC services; many District Hospitals do not provide VSC services year-round; and historically, mobile services have been focussed only on VSC and have not offered other methods. Factors contributing to these gaps include limited trained and skilled human resources, and supply issues. There is also insuffic-ient systemic focus on the provision of quality, client friendly, and comprehensive FP services, including comprehensive FP counselling, as assessed by the National Health Training Center quality improvement tools.
Auxiliary Nurse Midwives (ANMs) are the only service providers eligible to offer IUCDs at Health Posts and Birthing Centers; however, many have never received training, and those that have may not actually deliver services at their posts due to stock-outs of commodities, lack of equipment, and low client flow. A very limited number of eligible providers (including doctors, nurses, and ANMs) have received IUCD and voluntary implant insertion training.
Improving access to contraception has largely remained an effort contained within the health sector. Integration is a powerful way to reach women, men, and youth who may not otherwise seek Reproductive Health (RH)/FP care, but whose RH/FP needs may be especially great. When health and non-health agencies include RH/FP services and/or information in their programs, the resulting increase in the number of service delivery points leads to fewer missed opportunities, greater continuity of care, increased RH/FP access, and the sense on the part of clients that services are responsive to and respectful of their needs. Integrating FP into non-health-sector development projects, private institutions, cooperatives, and recently the Ministry of Health (MoH) test of introducing FP in the immunization programme could be effective ways to facilitate access to FP and other health services and information for women and communities. More evidence is needed on whether and how such efforts can work, and what types of models might be replicated and scaled up. The described study provides an early and unique look at the effectiveness of TICA in a non-health sector program for increasing FP utilization.
The study examines FP utilization in fifteen Village Development Committees (VDCs) of three districts: Rupandehi, Palpa, and Kapilvastu of the Western Development Region of Nepal, where an agriculture program was being implemented. TICA was designed to leverage community access points and resources of the localized agriculture program to address FP needs and challenges in the targeted areas. The TICA activities were concentrated in five of the VDCs in each of the three districts.
The TICA activities focused on increasing access to and demand for FP services through enhancing FP knowledge and demand generation activities such as:
Moreover, TICA utilized existing health and non-health structures, including health facilities, female community health volunteers, cooperatives, women’s groups, and adolescent groups. Building on the women’s groups, cooperatives, and market centers established and strengthened through the current Develop Local Economy to Eradicate Poverty (DEEP) project, TICA delivered FP education and services through peer education. Specifically, TICA delivered FP training directly to women’s groups after training group leaders. Cooperatives were engaged in managing mobile FP service camps in hard-to-reach areas, and also hosting and managing condom distribution boxes and question drop boxes, both of which were anonymously accessible by all community members. TICA also supported the upgrade of a selected number of health facilities through service provider training and material provision.
It was anticipated that improving utilization of FP would considerably increase Couple Year of Protection (CYP), and contribute to decreasing unwanted pregnancies and ultimately the Maternal Mortality Rate (MMR). TICA could also contribute to Nepal’s Sustainable Development Goals (SDGs) by supporting the private sector and MoH to increase availability of FP services and percentage of WRA utilizing FP methods. The objective of this evaluation was to assess 1) the effectiveness of a FP program focusing on increasing the utilization of LARC integrated into an agriculture (e.g., non-health) sector program, 2) the characteristics of clients visiting public health facilities in selected districts and their perspectives on the quality of FP services offered to them, 3) the level of awareness among clients on FP methods, and 4) knowledge and practice on access to and utilization of family planning methods.
The study design was descriptive cross-sectional (post intervention of the TICA Project). The study was carried out from November 2015 to February 2016 in five VDCs in each of three districts where an agricultural program was being implemented.
Settings: Palpa District is a mid-hill district in Western Nepal with a total population of 261,180 (male: 115,840; female: 145,340). Its CPR is 35.3%, slightly higher than the average regional CPR of 31.0%. Rupandehi District is in the Terai of Western Nepal with a population of 880,196 (male: 432,193; female: 448,003), and CPR is 31.6%. Kapilvastu District, also in the Terai, has a total population of 571,936 (male: 285,599; female: 286,337). Its CPR is 33.4%.8
The study population: The study population included married WRA, all of whom participated in the agriculture program (TICA Project Benefic-iaries). We did not include the same women groups in the baseline to minimize the bias. Women already sterilized before the implementation of TICA project were excluded from this study. The size of the sample was calculated as 25% of total agriculture program participants and 25% of the 60 existing women’s groups, i.e., 25% from 1800 (N) = 450 (n) among 15 women’s groups. However, the actual sample size was calculated as 525 from 21 women groups which included the 17% non-response rate. Samples were distributed according to the number of target beneficiaries that participated in the program of the 21 selected women groups.
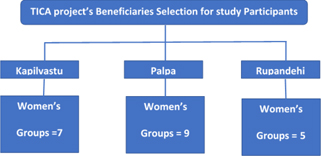
There was a total of 60 women’s groups within the agriculture program catchment area. A two-stage sampling technique was used to select respondents for participation in the study. In the first stage, of the 60 women groups a total of 21 groups were selected randomly from three agriculture program intervention districts. In the second stage, respondents within each group were selected by using a census method, i.e., all women from the 21 groups were included in the study. The study included 179 women from 7 women’s groups in Kapilvastu; 228 women from 9 women’s groups in Palpa, and 118 women from 4 women’s groups in Rupandehi (Figure 1). Data were collected through face-to-face interviews of the women (agricultural program beneficiaries) using semi-structured questionnaires during 18-30 November 2015.
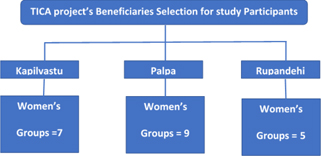
Figure 1: Diagram for sampling and sample size
Data processing included data entry program development, data entry, and data cleaning. EpiData software was used for data entry and analysis (version 3.1 for entry and version 2.2.2.183 for analysis, EpiData Association, Odense, Denmark) and validated before undertaking analysis. The data entered in EpiData was exported to SPSS and checked for inconsistencies. SPSS Descriptive was used for data analysis as per requirements. For multiple response data, where the respondents could choose or provide more than one response, multiple response analysis was done. The multiple responses were organized using multiple dichotomy (i.e., 1=yes and 0= no). The crosstab option was used to obtain frequencies or percentages according to the number of respondents/responses. For all continuous variables, the Shapiro-Wilk test for normality was used to check the distribution of data. When the test was significant (p value < 0.05) and suggested non-normal distribution of variable, a non-parametric test was used. The analyzed data was presented in tabular and graphical forms.
The baseline study was already accomplished in 2014/15 following same study design, cross-sectional descriptive. The sample size in the baseline study was 493 from 16 women groups, but the same women groups were not included in endline, e.g., women sterilized prior to implementation of the TICA project, to minimize the bias. Similarly, the same data collection tools were used for baseline and endline, i.e., data were collected from interviews, using semi-structured interview guidelines. Baseline data was collected before the intervention, whereas endline data were collected after the intervention. This report presents the comparative findings of both data collection points.
The research protocol was submitted to the Institutional Review Committee of ADRA Inter-national for ethical review and approval. Field works were commenced after obtaining approval from ADRA-I. A copy of the approval documentation was provided to all study sites. The consultancy team monitored for adherence to the research protocol and research norms and standards of ADRA International and Nepal.
Informed consent was obtained for participation in the survey. All the participants intending to take part in the survey signed a written consent form. All the participants’ related information was decoded and personal information was kept confidential and secured in the respective selected sites.
From the total of 525 WRA respondents, the average age was 32 years with a minimum age of 15 years and a maximum of 50 years. Nearly 25.0% of the sampled women did not live with their husbands as men commonly worked outside of Nepal. More than two-fifths (44.8%) of the women had informal education. Nuclear and joint (several households sharing a common kitchen) families were the predominant family systems. Agriculture was the main occupation, although some had been educated. Nearly 50.0% of women had income sufficient to feed their family for the whole year as shown in Table 1. “Disadvantaged” meant those who had been forced to fall backward politically, economic-ally, and socially; those who had been unable to avail services because of discrimination and harassment and because of geographical disconnection; and those communities whose standard of living had been below the legal standard as specified in the Human Development indicators.
Table 2 shows that almost all of the respondents (99.6%) had heard about FP. This means they were able to explain how to use FP methods, their side effects, and where to access them. Of these, more than two thirds (67.8%) correctly understood FP benefits as, among others, a method to prevent unwanted pregnancy. A sizeable number (other) understood FP to reduce unsafe abortion, limit family size, improve quality of life, and reduce the fertility rate. Most sources where respondents got information that was considered accurate about FP services were women’s literacy groups, Female Community Health Volunteers (FCHVs), school teachers, and health workers. Women also sought information from relatives/neighbors/friends. Study findings show that print material about FP was less effective in reaching the study participants as shown in Table 3.
Table 4 shows the percentage of women aware of various FP methods. The level of awareness for short-acting methods was higher compared to long-acting and permanent methods. The majority of respondents agreed that the upgrade of health facilities as FP sites, and the use of the drop boxes for FP questions and suggestions contributed to their increased awareness and knowledge of FP. Approximately three fourths (72.3%) of respondents said that government health institutions had been providing FP services to reach marginalized and disadvantaged groups as shown in Table 5.
The main FP methods used by the participants are presented in Figure 2. About half (47.6%) of the respondents reported using FP methods at the time of data collection. The contraceptives commonly used were Depo Provera and Minilap. The study found a significant decline in the proportion of women using short-acting methods from ever used to currently using, while, as expected, long lasting and permanent methods were found to have no significant difference. For example, the proportion of women using Depo Provera reduced drastically from 30.7% ever used to 10.3% currently using while the percentage of women ever used and currently using Minilap remained almost constant (13.0%).
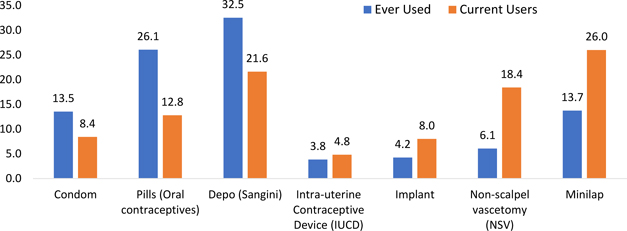
Figure 2: Comparative chart of status of ever used and current users of FP method by spouses (%)
Tables 6 and 7 show uptake of FP services by couples, as reported by respondents, stratified by age categories and educational level. There is low uptake of all methods of FP below age 20. Vasectomy was the most commonly used contraceptive method among couples with lower educational levels (non-schooled/informal, primary, secondary only) while Depo Provera for women was commonly used by couples with higher educational status (beyond secondary education).
Figure 3 shows that decisions on participating in FP and the choice of FP methods were predominantly made by the husband (68.0%) while men accompanied by women in making FP decisions is 32%. About a fifth (20.0%) of women reported that they were paying for FP services as shown in Figure 4. “No pay” status means that transportation costs and wage compensation were provided while utilizing services from health facilities. Table 8 shows that 68.4% of respondents reported that they were motivated by their husbands to use FP. Also, the study found that although the percentage of wives willing to utilize FP was higher than husbands (54.9% vs. 15.6%), the proportion of husbands willing to use FP saw an increasing trend after TICA interventions as indicated in Figure 5.
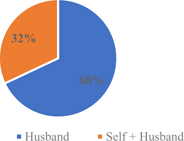
Figure 3: Decision Made on Using FP Methods (n=250)
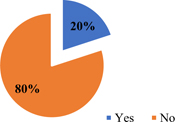
Figure 4: Pay Status for Using FP Methods (n=250)
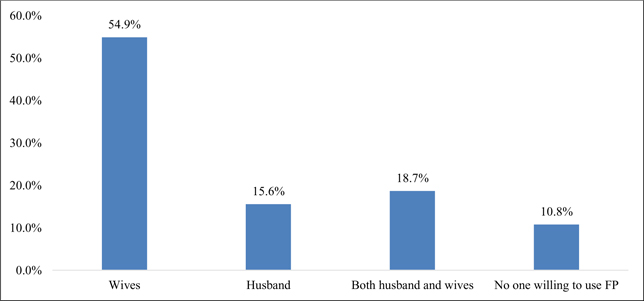
Figure 5: Willingness to Use FP Methods (n=406)
The reasons for not using FP devices were explored among the respondents who were not using any types of FP devices at the time of the study. The main reason identified (88.8%) was that their husbands were not living with them. Moreover, in Nepal, when women lived with their husband, they use FP methods. After husbands left to work outside of Nepal, then, the majority of women stopped using FP methods. Table 9 shows that in a smaller proportion of woman, lack of awareness, shyness about using the device, and/or lack of availability at the proximity were identified as the main reasons for not using FP devices.
Women perceived the optimal gap between births to be 48 months/4 years. Most of the women (98%) reported that FP helped to enhance their quality of life. Most of the women agreed that establishment of FP counselling and implant service rooms at local health facilities increased the quality of the FP services they received. Nearly all (97.0%) were satisfied with the FP services provided at the FP camps as shown in Figure 6 and Table 10.
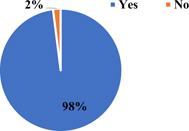
Figure 6: Perception that Family Planning Has Increased Quality of Life
A summary of findings comparing endline and baseline is shown in Tables 11 and 12. Overall, there has been an augmentation in knowledge of FP among study participants. Almost all of the participants had heard about FP at both baseline and endline. A statistically significant proportion (p=0.03) of endline participants had a correct understanding about FP. There has been a statistically significant increase in the proportion of women who had heard about at least four types of contraceptives by the endline compared to the baseline. A statistically significant improvement (p= 0 .001) in the practice of FP was achieved by the endline in terms of the proportion of couples ever using any FP methods.
| Feature Measured | Baseline (n=493) | Baseline (%) | Endline(n=525) | Endline (%) | P value |
|---|---|---|---|---|---|
| Knowledge of FP (No response=2) | 490 | 99.8 | 521 | 99.6 | |
| Women who correctly understand about family planning | 301 | 61.4 | 356 | 67.8 | P=0.03 |
| Heard of four types of contraception | 296 | 60.0 | 420 | 80.0 | P<0.001 |
| Spouse ever used any family planning | 360 | 73.0 | 426 | 81.1 | P<0.001 |
| Spouse currently using any family planning method | 256 | 51.9 | 263 | 50.1 | |
| Husbands willing to use FP | 17 | 5.2 | 63 | 15.5 | P<0.001 |
| Discussion about family planning with husband | 414 | 84.0 | 457 | 87.0 | |
| Women aware of short-acting FP methods | 424 | 86.0 | 485 | 92.3 | |
| Women aware of long-acting FP methods | 240 | 48.7 | 323 | 61.5 | P=0.016* |
| Women aware of permanent FP methods | 192 | 39.0 | 274 | 52.2 | |
| Spouse using permanent methods | 74 | 31.1 | 111 | 44.4 | |
| Satisfaction with the overall behavior of the health workers (Baseline n=322 and Endline n=420) | 316 | 98.1 | 415 | 98.8 | |
| Comprehensive counselling not practiced by HWs while providing FP Methods | 241 | 48.9 | 154 | 29.3 | P<0.001 |
| *Chi Square of three rows with data on awareness of short, long and permanent methods | |||||
The willingness among husbands to use FP methods substantially increased from 5.2% to 15.6% compared to baseline: the difference was statistically significant (p<0.001). In both baseline and endline, the majority of the respondents discussed FP with their husbands with the proportion being slightly increased over baseline. The percentage of respondents aware of short-acting FP methods increased from 86.0% to 92.3% post-intervention. The percentage aware of long-acting and permanent FP methods increased from 48.7% to 61.5% and 39.0% to 52.2%, before and after the intervention, respectively. The trend towards increased awareness of all three types of methods was significant. The proportion using permanent methods increased from 31.1% before the intervention to 44.4% after the intervention. There was no statistically significant difference (p= 0.10) in women between baseline and endline in terms of their opinion that FP methods helped to improve their quality of life.
There was statistically no difference among respondents on their satisfaction with various health facilities as well as health workers. Almost all of the respondents expressed that the overall behavior of the health worker towards them as the client appeared satisfactory at both baseline and endline. However, a statistically significant proportion of women at the endline (p< 0.001) expressed that more comprehensive counselling was given by health workers while providing FP methods.9
More specific evidence that improved knowledge translated into behavior is seen in Table 12. If the methods of contraception are grouped into temporary (condom, pill), long term/reversible (depo, IUD, implant), and permanent (vasectomy, minilap), there is a significant trend (p<0.001) towards employment of permanent methods.
The study of TICA activities demonstrates the feasibility of integrating FP into agricultural and potentially other non-health sectors. Evidence from the study suggests that TICA activities helped augment the knowledge of FP among the project population. The use of FP increased among agricultural program participants as a result of TICA, with a gradual shift from short-acting FP methods to long-acting and permanent FP methods. This was particularly true for the number of couples that used vasectomy as a FP method, which more than doubled at the end of the study period and was the most common FP method among the least educated couples. Also, this research showed that utilization of FP services could be increased through increased FP knowledge diffusion and awareness creation, with a high probability of encouraging husbands to use FP and be actively involved in FP decisions. Overall, the TICA activities were very successful in increasing FP knowledge level as well as promoting the use of FP among the targeted women.
Findings from a similar study show that integration was effective at increasing beneficiaries’ understanding and appreciation of the benefits of voluntary family planning. Further, beneficiaries perceived the program positively and reported an increase in acceptance of family planning as well as a decrease in myths and misconceptions about family planning.10
Another similar study revealed that about four of five women (81%) were currently using a modern contraceptive method. The most popular methods being used were injectables (38%) and pills (17%), followed by the intrauterine device (9%). Within the intervention group of 800 women, FP use for all methods increased significantly from 40% at baseline to 69% at endline, with a majority of new users.11
There is, however, room for improvement. The proportion of women who could not correctly explain FP and used short-acting FP methods, although substantially reduced at the study endline, remained quite high and emphasized the need for more awareness creation and FP sensitization.
The findings and conclusions are limited to the intervention group only and may not reflect the FP behaviors of the entire district population. According to TICA program reports, nearly 25% of the sampled women’s husbands were working outside of Nepal. This may have impacted and most likely reduced the proportion of women currently using FP as well as limited the potential for women to discuss FP with their husbands. Follow up questions were not asked among those women who said that the main reason they did not use FP methods was that they were not living with their husbands; if their husbands return intermittently, this data may not be accurate.
Integrating FP activities with non-health sector interventions is acceptable to communities, engages males and youth, and tends to increase community goodwill toward other aspects of the project that may not originate as community priorities. Including FP activities in livelihoods interventions can increase community support for programming whose benefits are longer-term and increase resonance among men, women, and youth, potentially increasing their involvement and support for activities.
It was discouraging to see that the willingness among husbands to use the FP method was still low (15.5%). Thus, males should also be encouraged to participate in family planning issues. Male involvement in FP should be the area of action and research in future. It is recommended that similarly integrated FP programming be replicated in the study districts as well as other districts in Nepal. Since this community approach worked, it could be tested for implementation through other community structures in addition to cooperatives, women’s groups, men’s groups, and youth clubs.