ORIGINAL ARTICLE
A Study of Volunteer Community Health Workers Promoting Maternal Health Services in Rural Kenya: A Christian Viewpoint
Bradly Alexander Kimbrougha and Lisa Bakerb
Abstract
Introduction: Despite the call for community-based health care interventions in the developing world, there is little research examining the effectiveness of paid versus volunteer community health worker (CHW) programs to increase women’s use of maternal health services. From a Christian perspective, the CHW model is, at its root, discipleship: a credible person leads a neighbor to a source of help and health. This effective model can be expanded to address the health of the whole person, both spiritual and physical. This study of a government health center program in rural Kenya addresses these issues.
Methods: The current study analyzed the change in maternal health services after a government program, starting with 30 volunteer CHWs, had been in place for nine months. The intervention was designed and carried out by the authors in collaboration with Sigoti District Health Center in the western Kenyan province of Nyanza.
Results: The proportion of facility-based deliveries (FBDs) showed a statistically significant increase (p=0.003), from an average of 38 deliveries before the intervention to 60 afterwards. The proportion of health center deliveries of HIV-positive women also significantly increased (p=0.04) from an average of 6.5 to 14 FBDs. Compared to another program in rural Lesotho with paid CHWs, the Sigoti intervention led to a similar increase in FBDs. Despite their successes, the community-based strategies were time-intensive for both programs, with one CHW adding between 1.12 and 1.7 FBDs per year.
Discussion: This study demonstrates that a CHW program can be successful, even when using volunteers. Using solely a metric of time and/or money, the CHW model produces value at a high cost. However, the concerns of cost-effectiveness and CHW attrition, as well as the success of the CHW model, can be meaningfully addressed from a Christian perspective. Using the outcome measure of changed lives, volunteer CHWs could be motivated by a Christian call to discipleship. CHWs may be trained and supported to contribute to the health of the whole person. Future research will test these assumptions with a CHW program operating from a Christian health center to be built soon in the study area.
Introduction
The challenge of disease and death in the developing world has provoked a variety of responses from the international community, including grants of billions of dollars from development agencies, the investment of thousands of overseas micro-loans, and government interventions to build health care infrastructure. All of these approaches have brought some success, and widespread systemic change is essential to address the complex issues of health today that are inextricably linked with poverty and social injustice.
On the other hand, a response that is deeply personal and local is the popular strategy of using community health workers (CHWs) in their own neighborhoods to encourage individuals to access health care and to teach the means of health promotion. Since the Alma-Ata Declaration in 1978, CHW programs have become a key element in maternal and child health. The CHW model later became an essential strategy in working toward the fifth Millennium Development Goal (MDG) of having 80% of births take place with skilled personnel.1 In another aspect of maternal and child health, CHWs have been utilized to reduce mother-to-child transmission of HIV,2,3 which can potentially be decreased to less than 2% with the appropriate use of anti-retroviral therapy (ART).4
This approach of affecting one person at a time in the context of a personal relationship is precisely what Jesus modeled throughout his ministry. It is not surprising that CHWs have been well received and are believed to be successful. However, there remains a dearth of evidence to support the claims of success and cost-effectiveness of CHW programs.5,6,7,8 Outcome studies that do exist generally focus on CHW programs aimed at health promotion,9 tuberculosis care,10,11,12,13,14,15 and immunization services.16 Consequently, in 2013 the World Health Organization (WHO) called for a comprehensive research effort on the efficacy of CHW programs.17
The effectiveness of CHWs in reaching pregnant women is still largely unknown. Two major studies have addressed this gap by evaluating CHW programs in Sub-Saharan Africa.18,19 In an attempt to achieve the MDGs, the country of Ethiopia initiated the Health Extension Program in 2003. With approximately one salaried worker for 2500 residents, there was a documented increase in antenatal care (ANC) and family planning after the program was instituted, but the proportion of women delivering at a health facility did not change.18 In a more comprehensive effort that employed a much higher concentration of CHWs than in the Ethiopian study, a program was instituted in a highland region of Lesotho where 46 deliveries per year (out of a population of 25,000 in the catchment area) were occurring at a local facility. Traditional birth attendants (TBAs) were retrained as CHWs by the non-profit organization Partners in Health.19 The catchment area was served by one hundred CHWs (a ratio of 1 to 250, i.e., ten times more workers per population compared to the Ethiopian intervention) who were paid an incentive-based salary equivalent to approximately $36 USD per month (extrapolated from original article using the exchange rate at the time of the study).19 Notably, the CHWs were part of a multi-faceted approach to increase utilization that also included the establishment of a maternal “waiting house” where pregnant women could go and receive three meals a day for up to two weeks prior to their due date. The combination of these changes showed an increase from 46 to 178 facility-based deliveries in the first year and 216 in the second year of the program. During the two-year intervention, 55% of the women who delivered at the facility took advantage of the opportunity to stay in the maternal waiting house. It is unknown how much of the improvement was due to the CHWs versus the benefits of the maternal waiting house.
Broader approaches of examining the cost-effectiveness of CHWs that include relational changes and changes in behavior have generally not been well recognized,5 though in recent years there has been an increase in this literature.20,21,22 One such study was of a community-based midwifery program that evaluated whether perinatal outcomes and ANC attendance improved in addition to other factors, such as empowerment and family-centered care.20 Though the quantitative improvements were negligible in the midwifery study, the qualitative results were quite positive.
The current study took place among a community of Luo people living on the Nyakach Plateau in the Nyanza Province of western Kenya, a destitute area of rocky dirt roads, inadequate subsistence farming, no dependable clean water source, no sanitation services, and little health care. Kenya ranks fourth in the world in the number of people living with HIV/AIDS, 23 and women of the Luo tribe of western Kenya have the highest HIV rate (22.8%) and the highest infant mortality (9.5%) in the country.24 Kenya’s maternal mortality has been volatile over the last twenty-five years. In 1990, the maternal mortality rate was 380 per 100,000 births, but in 2005, it increased to 580/100,000.25 As of 2013, the rate decreased again to 360/100,000,26 a figure that is still alarming and does not meet the fifth Millennium Development Goal (MDG) of reducing maternal mortality by 75%. One issue driving the high maternal mortality is that only one-third of women living in rural Kenya give birth with skilled personnel.24 Some locations in Kenya have a rate as low as 5.4%,27 in spite of the fact that skilled birth attendance has been deemed as the most important factor in preventing maternal deaths.28
On the Nyakach Plateau, the local government district health center (Sigoti Health Center) is staffed by a clinical health officer and two nurses who have had great interest in increasing maternal services. One village in the catchment area is East Koguta (referred to as a “sub-location” in Kenya) with a population of 7360 and an estimated 260 births a year, 59 of them to mothers with HIV.24 Approximately 19% of those births and 15% of the HIV deliveries were occurring at the Sigoti Health Center up to mid-2011. This health center has no resources to pay CHWs. However, the clinic personnel appreciate the value of the CHW model and decided to experiment by training volunteers who wanted to contribute in a meaningful way and invest deeply in their own community. Data suggest that sustainable success depends on salaries and other monetary incentives,29 yet these leaders believed that their consistent, supportive relationships with the workers, combined with simple incentives of food and help with travel, would be enough to make a difference. They hoped that financial resources might emerge at some point, but they decided to see if the workers would participate based on the value of the expertise they gained and the satisfaction of doing an important task. Thirty people from East Koguta volunteered to work with their own neighbors to identify needs and serve pregnant women. More than two-thirds of these workers stayed with the program for its first nine months.
Methods
East Koguta Community Health Worker (EKCHW) Program
Over a two-week period in August of 2011, a public health officer and the head nurse from the Sigoti Health Center trained thirty volunteer CHWs (twenty-nine women and one man) according to the International Center for AIDS Care and Treatment Programs (ICAP) at Columbia University’s Mailman School of Public Health. The requirements for becoming part of the EKCHW Program were to have at least a fourth-grade education and to be a respected community member. The CHWs were predominantly Christian and served in a part of Kenya that has been traditionally Christian for many years. However, this government program did not deliberately attempt to recruit Christians or to frame their activities in a Christian context.
The East Koguta CHWs were trained to provide health education for pregnant women, encourage them to go to ANC visits, and urge them to deliver their babies at the health center instead of at home or with a TBA. HIV-positive mothers and other high-risk pregnant women were especially targeted and encouraged to deliver at the health center. The Sigoti Health Center goal was to increase the number of facility-based deliveries from 19% (the rate prior to the program) to 30% of all births occurring within the area.
Maternal health services were a primary focus of the CHW program, but the workers were also trained to conduct a variety of other tasks: tracking former patients for check-ups, bringing HIV-positive patients to the health center who had neglected to receive treatment, health education, and identifying and referring community members with suspected illnesses such as malaria, tuberculosis, and HIV-associated illnesses.
During nine months of implementation, eight women discontinued volunteering. According to the head of the EKCHW Program, the main reason for volunteers dropping out was unrealized hopes of future wages, while the main reason for deciding to continue was the CHWs’ “heart” for the community. The CHWs met weekly with the public health officer and head nurse. The CHWs were expected to work an average of two to three hours a day beginning in September of 2011. The only compensation for the workers was an occasional free meal or refreshment, use of a communal bicycle, and informal community recognition.
Analysis of health records
The current study analyzed health center records from the Sigoti District Health Center located in the Nyanza Province of Kenya. The data included information about all women from East Koguta who delivered at the health center from September 2009 through May 2012. The original information was collected and entered by hand into the record by the nurses or the clinical officer at each ANC visit and at the time of delivery. Relevant data were later copied from the medical record by a trained research assistant and were then coded and transferred into an Excel spreadsheet for analysis.
Data from a nine-month period (the first of September to the first of June) for the two years prior to the intervention were compared to the same nine-month period during the intervention year (see Figure 1).
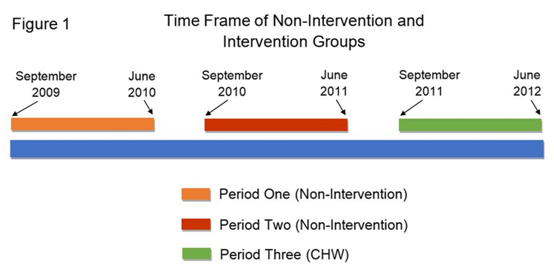
These three time periods are referred to as Period 1, Period 2, and Period 3 (CHW), respectively. The most recent available regional data were used (DHS 2008-2009 for crude birth rate and 2009 Kenya census data for population statistics)24 to compare the Sigoti Health Center numbers with the number of women who gave birth in the entire area (sub-location of East Koguta) during the timeframe of the study. Given the crude birth rate and the number of people living in East Koguta, the number for a nine-month period was extrapolated to yield 195 deliveries. The number of deliveries was estimated using the following equation: Number of Deliveries = [CBR*(Pop/1000)]*0.75. The CBR is the crude birth rate for the area (Kenya DHS 2008-2009), Pop is the population of East Koguta, and the total was multiplied by 0.75 to yield the estimated number of deliveries in nine months.
The number of births from HIV-positive women during a nine-month period was estimated by multiplying 195, the estimated number of deliveries, by the HIV-prevalence among Luo women, 0.228, giving an estimate of 44 HIV-positive women delivering in East Koguta over a nine-month period. 24
Data from Periods 1 and 2 were combined and compared with Period 3 (CHW) to determine if the intervention significantly increased the number of facility-based deliveries, the number of HIV-positive women who delivered at the facility, and the number of women who received the 4+ ANC visits recommended by the World Health Organization. The mean, standard deviation, and range for continuous variables are reported, and the frequencies, proportions and percentages are reported for categorical variables. The Chi-square and t statistics were used to test differences from before and after the intervention for discrete and continuous variables, respectively. Alpha was set at .05. Statistical analyses were done using the statistical software SAS 9.2 by SAS Institute Inc. (Cary, North Carolina).
Results from the current study were then compared to data from the more comprehensive, salaried CHW program in Lesotho19 to determine if this volunteer program was as effective in achieving positive results.
Ethical considerations
This study was approved by the Baylor University Institutional Review Board and was exempt from the requirement for informed consent, as it was a study of anonymous subjects with information drawn from previously collected clinical data. During the research process, no patient names were associated with any of the data. The names of individual patients were not recorded in the research database.
Results
Sample characteristics
The mean age and parity of women delivering at the health center during Period 3 (CHW) were not significantly different than women in Periods 1 and 2 (see Table 1). During each time period, about a quarter of all deliveries were by first-time mothers. Every woman attended at least one ANC visit.
Table 1. Sample Characteristics Before and After East Koguta CHW Program| Variable | Mean (SD) | t | p |
| AGE | 0.17 | 0.87 | |
| Periods One and Two | 22.66±5.07 | ||
| Period Three (CHW) | 22.81±5.78 | ||
| PARITY | 0.94 | 0.35 | |
| Periods One and Two | 1.70±1.72 | ||
| Period Three (CHW) | 1.98±1.74 |
Results of the intervention
The data for the three outcomes of interest are presented in Table 2.
Table 2. Comparison of Three Outcomes Before and After the East Koguta CHW Program| Variable | Proportion | Percentage | Chi-square | p |
| DELIVERIES | 8.65 | 0.003 | ||
| Periods One and Two (Combined) | 76 / 389.7 | 19.5 | ||
| Periods One and Two (Average) | 38 / 194.9 | 19.5 | ||
| Period Three (CHW) | 60 / 194.9 | 30.8 | ||
| HIV-POSITIVE | 4.23 | 0.04 | ||
| Periods One and Two (Combined) | 13 / 88.9 | 14.6 | ||
| Periods One and Two (Average) | 6.5 / 44.4 | 14.6 | ||
| Period Three (CHW) | 14 / 44.4 | 31.5 | ||
| 4+ ANC VISITS | 3.47 | 0.06 | ||
| Periods One and Two (Combined) | 19 / 389.7 | 4.9 | ||
| Periods One and Two (Average) | 9.5 / 194.9 | 4.9 | ||
| Period Three (CHW) | 18 / 194.9 | 9.2 |
There was at least a 50% increase in all three outcomes: number of facility-based deliveries (58% increase), number of HIV-positive deliveries (115% increase), and number of women with 4+ ANC visits (89%). The Sigoti Health Center did, in fact, reach its goal of having 30% of the actual number of catchment area deliveries occurring at the clinic after the intervention began. When comparing the combined number of facility-based deliveries in Periods 1 and 2 (76 out of 390 expected deliveries) to the number in Period 3 (CHW) (60 out of 195 expected deliveries), the change after the intervention was statistically significant (p=0.003). The increase in the proportion of HIV-positive women delivering was also statistically significant (p=0.04). More HIV-positive women delivered during the intervention than in Periods 1 and 2 combined. The number of women receiving 4+ ANC visits during the intervention also increased from an average of 9.5 women (Periods 1 and 2) to 18 during the intervention. However, even with this substantial increase, the small sample size did not provide enough power to achieve statistical significance, though it was close (p=0.06).
Despite these encouraging results, it is sobering to note that over two-thirds of HIV-positive women in the area did not deliver in the health center, and less than 10% of women were receiving the recommended number of ANC visits, even during the intervention. Part of the explanation lies in the difficult geographical environment in which these women live. Health care services are delivered sporadically due to periods of flooding and drought that make travel difficult for patients and for those delivering supplies to the clinic. A pattern of monthly variation exists each year in the number of deliveries, as shown by Figure 2.
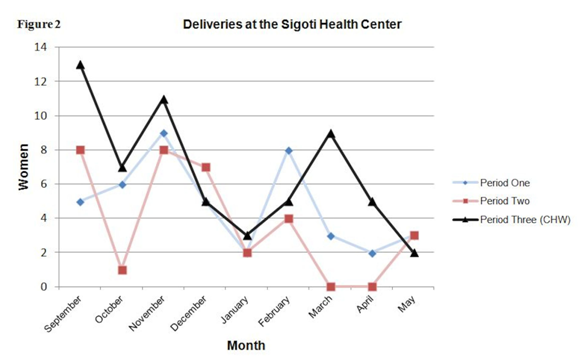
Peaks in the number of deliveries occurred in the months September, November, and February while troughs occurred in the months October, January, and May. Dirt roads are rough or nonexistent, almost no one has transportation other than walking, and most women have many children to care for. A trip to the health center for an HIV-positive, pregnant woman with toddlers can be challenging in the best weather. In periods of flooding, during active labor, and perhaps at night in an area with no lights, this journey may be impossible.
Comparison of East Koguta and Lesotho CHW Programs
A comparison of this study’s data with the success of the Lesotho CHW program19 is shown in Table 3 below. The Lesotho program had a baseline of far fewer facility-based deliveries (6.8% vs. 19% in East Koguta). With their interventions, however, both programs achieved the same results, i.e., approximately 30% of deliveries occurring at the health facility. East Koguta went from 19.5% to 30.8%. Lesotho increased from 6.8% to 26.3% in year 1 and to 31.9% in year 2, an average of 29.1% facility-based deliveries. The two programs had a comparable ratio of CHWs to the population (one for every 250-283 residents).
It is unknown how much of the improvement in Lesotho was due to the addition of CHWs and how much was a result of the establishment of the maternal waiting house. In the East Koguta region, where people rarely eat more than one meal a day and women must walk an average of 3.8 kilometers to the health center, such an opportunity would be not only an incentive, but sometimes would be life-saving.
Table 3. Comparison of East Koguta and Lesotho CHW Programs| Population | CHW Salary | Number of CHWs | CHWs per Population | Additional FBD per CHW per Year | |
| East Koguta | 7360 | None | 26 * | 1 / 283 | 1.12 |
| Lesotho (yr 1) | 25000 | About US $36 per month | 100 | 1 / 250 | 1.32 |
| Lesotho (yr 2) | 25000 | About US $36 per month | 100 | 1 / 250 | 1.70 |
| Non-Intervention | Number of FBD | Percentage of FBD per Total Deliveries | |||
| East Koguta | 51 | 19.5% | |||
| Lesotho | 46 | 6.8% *** | |||
| Intervention | |||||
| East Koguta | 80 ** | 30.8% | |||
| Lesotho (yr 1) | 178 | 26.3% | |||
| Lesotho (yr 2) | 216 | 31.9% | |||
In East Koguta, one CHW produced an average of 1.12 additional facility-based deliveries per year (extrapolated from nine months). In the Lesotho study, the yield was slightly higher — one CHW (plus the maternal waiting house) produced an average of 1.32 additional deliveries during the first year and 1.70 additional deliveries the second year. This better result was achieved with a slightly more favorable ratio of CHWs to population residents (1:250 in Lesotho vs. 1:283 in East Koguta). With an approximate cost of $432 (US) per year for a Lesotho CHW, the cost of bringing in one additional woman to deliver in the health center is between $327 (year 1) and $254 (year 2). In terms of cost-effectiveness, this strategy is relatively expensive and extremely time-intensive. In contrast, if the CHWs are volunteers and if the health center can absorb the lost workdays of the trainers, then the intervention easily becomes financially cost-effective, though still quite costly in terms of the time invested by the workers.
The Lesotho program, with paid CHWs, did not show vastly different results from the East Koguta volunteer program. However, the Lesotho program also included the excellent resource of the maternal waiting house used by over half of the women in addition to the CHW intervention. The cost of the waiting house is not reported, but it is likely to have substantially increased the cost of the program per woman delivering at the health center.
Discussion
Success, sustainability, and cost-effectiveness: A Christian viewpoint
This study provides evidence that volunteer CHWs can be effective in increasing the number of facility-based deliveries, especially for HIV-positive women, and the results are encouraging for increasing the number of women with the recommended 4+ ANC visits. It is striking that this impact was achieved by volunteers in a highly challenging physical environment within only nine months. In fact, the onset of the program’s impact was rapid. Within the first few months, there was already a noticeable difference in the number of facility-based deliveries compared to the same months from previous years. It is also promising that this program was just as effective, at least in the short run, as a CHW intervention in a comparable rural African setting that had financial incentives for CHWs and a “waiting house” for pregnant women.
Viewed another way, what is notable about the results from the current study is that so many East Koguta CHWs did continue to volunteer with no financial incentive. The Sigoti Health Center staff believes that success has been due to: close contact between the CHWs and the health center personnel, non-monetary rewards that are meaningful, and early feedback to the CHWs about the apparent success of the program (personal communication, March 2013). Also, the East Koguta intervention was generated and implemented by residents of East Koguta, instead of being imposed by the government or by an outside organization. Another contributing factor was believed to be the important support from the local TBAs, and an increased role for them is possible in the future.
A Christian is not surprised at the success of a CHW model, because the method is the same as that used by Jesus in his work of discipleship. Neither is a Christian discouraged by threats to sustainable motivation for volunteers or by work that is extremely time-intensive in producing results. The approach of Jesus was not to create institutions, but to empower his followers to share the good news with one person at a time. He sent them out with instructions to travel light, meet the needs of the whole person, and spend time with those who have ears to hear and eyes to see. “When you enter a town and are welcomed, eat what is set before you. Heal the sick who are there and tell them, ‘The kingdom of God is near you’” (Luke 10:8-9, NIV). An effective CHW is one who shares her experience with someone she knows and brings that person along with her to the next level of understanding. An effective follower of Christ does the same.
The positive results from the current study and the Lesotho study are tempered by the questions they raise about sustainability and cost-effectiveness. Having volunteer CHWs may answer the troubling challenge of paying salaries, but it is unknown how much worker attrition over a longer time period would affect success. The positive outcomes achieved in the first nine months of the East Koguta CHW program were accompanied by an average attrition rate of about one CHW per month. It is possible that relying on volunteers is only productive for a short time, regardless of how meaningful the work is. Further research can evaluate this issue. No attrition among the paid CHWs in the Lesotho program is reported, so it is impossible to compare this aspect of the two programs. The omission in the description of the Lesotho program may indicate no attrition, but it is more likely that the number of CHWs was maintained by replacing any CHWs who left with new paid workers.
To the degree that a volunteer CHW program is framed as meaningful Christian service, it can be maximally sustainable. As this government program did not attempt to frame the work in a Christian context, the attrition of CHWs suggests that altruism alone is not enough to sustain some volunteers. However, it is our belief that volunteers can be uniquely and successfully motivated by a Christian call to the healing of the whole person accompanied by formation and support for that task.
The other concern raised by this analysis is that a program that takes one worker eight to twelve months to yield one facility-based delivery is not likely to be judged as cost-effective by most organizations. Still, when unemployment is high and CHW activities can be meaningful, the volunteer CHW strategy remains viable. This is the case when a cost-benefit analysis is restricted to an outcome of increased facility-based deliveries. A more convincing case may be made if broader outcomes are considered. It has been said that ”examples of wider benefits may result from CHWs that are unlikely to be captured in cost-effectiveness analysis are employment and training opportunities, the value attached by clients to the process of receiving such services, and institutional change,“ where institutions are described as: “the patterns of behavior that determine how individuals, groups and organizations interact with one another.”5
If the desired outcomes are expanded even further and the health that is sought is spiritual as well as physical, the volunteer CHW model may be the most effective investment of time that can be made to achieve those goals. For a Christian, the “cost” of discipleship is life itself, and the “benefit” is the kingdom of God. This perspective brings a new meaning to concepts of success, volunteerism, and cost-effectiveness. The CHW strategy can be supported — not in spite of, but because of its time-intensive nature — when the task is expanded to address the health of the whole person.
If the desired outcomes are expanded even further and the health that is sought is spiritual as well as physical, the volunteer CHW model may be the most effective investment of time that can be made to achieve those goals. For a Christian, the “cost” of discipleship is life itself, and the “benefit” is the kingdom of God. This perspective brings a new meaning to concepts of success, volunteerism, and cost-effectiveness. The CHW strategy can be supported — not in spite of, but because of its time-intensive nature — when the task is expanded to address the health of the whole person.
There is a spiritual and material component to every structure, even when it is not created with a spiritual focus in mind. From a Christian perspective, the physical health of the community cannot be the centerpiece of an intervention to the exclusion of the spiritual, nor can the spiritual be the center to the exclusion of the physical. Jesus said about his own purpose, ”The Spirit of the Lord is on me, because he has anointed me to preach good news to the poor. He has sent me to proclaim freedom for the prisoners and recovery of sight for the blind, to release the oppressed, to proclaim the year of the Lord’s favor.“ (Luke 4:18-19, NIV)
Community Health Evangelism (CHE), a model for community development and discipleship, is commonly used by Christian development organizations and churches.31 CHE trainers, generally under the supervision of a local church or mission agency, introduce CHE to their communities and train volunteers to teach lessons on preventive health and Christian discipleship. The East Koguta CHW Program differs from the CHE model primarily in two ways: it was established and supervised by a non-church entity, the local health center, and was created in response to very specific health problems, namely a high HIV prevalence and maternal/infant mortality. The models are similar in that both are formed and operated by community members in order to provide the community with ownership of the program.
Future efforts in the Luo community that is the setting of this study include building a new health center by a Christian non-profit organization (Straw to Bread) that has been working in collaboration with local residents in the area since 2001. This initiative, informed by data from the current study seen through a Christian lens, can move toward building a CHW program that is intentionally Christian in orientation. The volunteer CHW model is a great fit for those who are working to lead people toward spiritual as well as physical wholeness. A CHW who is also a follower of Christ could bring all of who she is to the role.
Following the example of Christ in teaching his followers, a CHW program built on Christian principles would enhance sustainability and the potential for success by placing heavy emphasis on training and encouraging the CHWs. The commitment of the trainers to the CHWs becomes the model for the commitment of the CHWs to the people with whom they work. Trainers for such a program would:
- Take seriously the formation process — invest deeply and develop relationships with and among the CHWs.
- Develop a common vision of the health of the whole person.
- Equip CHWs to bring hope, knowledge, and transformation to the whole person.
- Serve, encourage, and learn from the CHWs by listening, adapting, and continually revising plans based on input from those doing the work.
- Trust the CHW to deliver good news out of the strength of her uniqueness.
Summary
Based on the current study in rural western Kenya, a volunteer CHW program can be an effective means to increase the use of maternal health services. However, the inherent difficulties of sustaining a volunteer model and the cost-effectiveness of the labor-intensive CHW role make its usefulness questionable in the current context. Though the East Koguta CHW program does not have a Christian framework for recruitment, training, or management, we believe that a CHW program in a Christian context could provide the motivation and meaning required for sustainability and could provide transformational results to communities through relationships formed with a higher purpose. A CHW program within a Christian framework could be successfully carried out by volunteers who see their mission as the supreme joy of sharing good news at every level with all of their heart, soul, mind, and strength. With the mindset of Christian discipleship, CHWs can emulate the two-fold call of Christ to meet both physical and spiritual needs.
References
- Bhutta ZA, Ali S, Cousens S, Ali TM, Haider BA, Rizvi A, et al. Alma-Ata: Rebirth and Revision 6 Interventions to address maternal, newborn, and child survival: what difference can integrated primary health care strategies make? Lancet. 2008 Sep 13;372(9642):972-89. http://dx.doi.org/10.1016/S0140-6736(08)61407-5
- Boateng D, Kwapong GD, Agyei-Baffour P. Knowledge, perception about antiretroviral therapy (ART) and prevention of mother-to-child-transmission (PMTCT) and adherence to ART among HIV positive women in the Ashanti Region, Ghana: a cross-sectional study. BMC Women’s Health. 2013;13:2. http://dx.doi.org/10.1186/1472-6874-13-2
- Kim MH, Ahmed S, Preidis GA, Abrams EJ, Hosseinipour MC, Giordano TP, et al. Low rates of mother-to-child HIV transmission in a routine programmatic setting in Lilongwe, Malawi. PLoS ONE. 2013;8(5):e64979. http://dx.doi.org/10.1586/14787210.3.6.971
- McIntyre J. Prevention of mother-to-child transmission of HIV: treatment options. Expert Rev Anti Infect Ther. 2005 Dec;3(6):971-80. http://dx.doi.org/10.1586/14787210.3.6.971
- Walker DG, Jan S. How do we determine whether community health workers are cost-effective? Some core methodological issues. J Community Health. 2005 Jun;30(3):221–9.
- Prinja S, Mazumder S, Taneja S, Bahuguna P, Bhandari N, Mohan P, et al. Cost of delivering child health care through community level health workers: how much extra does IMNCI Program cost? J Trop Pediatr. 2013 Jul 19-057. http://dx.doi.org/10.1093/tropej/fmt057
- Prinja S, Jeet G, Verma R, Kumar D, Bahuguna P, Kaur M, et al. Economic analysis of delivering primary health care services through community health workers in 3 North Indian states. PLoS ONE. 2014;9(3):e91781. http://dx.doi.org/10.1371/journal.pone.0091781
- Lewin S, Munabi-Babigumira S, Glenton C, Daniels K, Bosch-Capblanch X, van Wyk BE, et al. Lay health workers in primary and community health care for maternal and child health and the management of infectious diseases. Cochrane Database Syst Rev. 2010;(3):CD004015. http://dx.doi.org/10.1002/14651858.CD004015.pub3
- Wang’ombe JK. Economic evaluation in primary health care: the case of Western Kenya community based health care project. Soc Sci Med. 1984;18(5):375-85. http://dx.doi.org/10.1016/0277-9536(84)90055-8
- Floyd K, Skeva J, Nyirenda T, Gausi F, Salaniponi F. Cost and cost-effectiveness of increased community and primary care facility involvement in tuberculosis care in Lilongwe District, Malawi. Int J Tuberc Lung Dis. 2003 Sep;7(9 Suppl 1):S29-37.
- Islam MA, Wakai S, Ishikawa N, Chowdhury AMR, Vaughan JP. Cost-effectiveness of community health workers in tuberculosis control in Bangladesh. Bull World Health Organ. 2002;80(6):445-–50.
- Nganda B, Wang’ombe J, Floyd K, Kangangi J. Cost and cost-effectiveness of increased community and primary care facility involvement in tuberculosis care in Machakos District, Kenya. Int J Tuberc Lung Dis. 2003 Sep;7(9 Suppl 1):S14-20.
- Okello D, Floyd K, Adatu F, Odeke R, Gargioni G. Cost and cost-effectiveness of community-based care for tuberculosis patients in rural Uganda. Int J Tuberc Lung Dis. 2003 Sep;7(9 Suppl 1):S72-79.
- Sinanovic E, Floyd K, Dudley L, Azevedo V, Grant R, Maher D. Cost and cost-effectiveness of community-based care for tuberculosis in Cape Town, South Africa. Int J Tuberc Lung Dis. 2003 Sep;7(9 Suppl 1):S56-62.
- Wilkinson D, Floyd K, Gilks CF. Costs and cost-effectiveness of alternative tuberculosis management strategies in South Africa--implications for policy. S Afr Med J. 1997 Apr;87(4):451-5.
- San Sebastián M, Goicolea I, Aviles J, Narvaez M. Improving immunization coverage in rural areas of Ecuador: a cost-effectiveness analysis. Trop Doct. 2001 Jan;31(1):21-4.
- Invitation to tender for the development of a ‘Cost-effectiveness study on community health workers.’. World Health Organization; 2013. Available from: http://www.who.int/workforcealliance/media/news/2013/GHWA_ITT_CHW_CEA_5Mar2013.pdf
- Medhanyie A, Spigt M, Kifle Y, Schaay N, Sanders D, Blanco R, et al. The role of health extension workers in improving utilization of maternal health services in rural areas in Ethiopia: a cross sectional study. BMC Health Services Research. 2012 Oct 8;12(1):352. http://dx.doi.org/10.1186/1472-6963-12-352
- Satti H, Motsamai S, Chetane P, Marumo L, Barry DJ, Riley J, et al. Comprehensive approach to improving maternal health and achieving MDG 5: report from the mountains of Lesotho. PLoS One. 2012 Aug 27;7(8). http://dx.doi.org/10.1371/journal.pone.0042700
- Jan S, Conaty S, Hecker R, Bartlett M, Delaney S, Capon T. An holistic economic evaluation of an Aboriginal community-controlled midwifery programme in Western Sydney. J Health Serv Res Policy. 2004 Jan;9(1):14-21.
- Jan S. A holistic approach to the economic evaluation of health programs using institutionalist methodology. Soc Sci Med. 1998 Nov;47(10):1565-72. http://dx.doi.org/10.1016/S0277-9536(98)00228-7
- Jan S, Pronyk P, Kim J. Accounting for institutional change in health economic evaluation: a program to tackle HIV/AIDS and gender violence in Southern Africa. Soc Sci Med. 2008 Feb;66(4):922–32. http://dx.doi.org/10.1016/j.socscimed.2007.11.010
- The World Factbook: Country comparison: people living with HIV/AIDS [Internet]. Washington, DC: Central Intelligence Agency; [updated 2012; cited 2014 Mar 10]. Available from https://www.cia.gov/library/publications/the-world-factbook/rankorder/2156rank.htmlKenya.
- Kenya National Bureau of Statistics, ICF Macro (2010). Kenya demographic and health survey 2008-2009. Calverton, United States: ICF Macro. Available from: http://dhsprogram.com/publications/publication-FR229-DHS-Final-Reports.cfm
- Chou D, Inoue M, Mathers C, Oestergaard M, Say L, Mills S, et al. Trends in maternal mortality: 1990 to 2008. World Health Organization, United Nations Children’s Fund, United Nations Population Fund, The World Bank; 2010. Available from: http://www.unfpa.org/webdav/site/global/shared/documents/publications/2010/trends_matmortality90-08.pdf
- Maternal mortality ratio (modeled estimate, per 100,000 live births) [Internet]. Washington, DC: The World Bank; [updated 2014 Apr 2; cited 2014 Apr 3]. Available from: http://data.worldbank.org/indicator/SH.STA.MMRT
- Cotter K, Hawken M, Temmerman M. Low use of skilled attendants’ delivery services in rural Kenya. J Health Popul Nutr. 2006 Dec; 24(4):467-71.
- Reduction of maternal mortality. A joint World Health Organization, United Nations Children’s Fund, United Nations Population Fund, and World Bank statement; 1999. Available from: https://extranet.who.int/iris/restricted/bitstream/10665/42191/1/9241561955_eng.pdf
- Community health workers: What do we know about them? World Health Organization; 2007. Available from: http://www.who.int/hrh/documents/community_health_workers.pdf
- Ministry of Health and Social Welfare (Lesotho), ICF Macro (2010) Lesotho Demographic and Health Survey 2009. Calverton, United States: ICF Macro. Available from: http://dhsprogram.com/publications/publication-FR241-DHS-Final-Reports.cfm
- What is CHE? [Internet]. Community Health Evangelism; [cited 2014 Oct 3]. Available from http://chenetwork.org/whatische.php