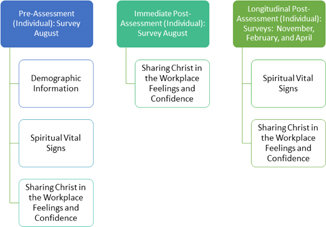
Figure 1. Timing of Assesments
ORIGINAL ARTICLE
Felisha L Younkina, Emily Laswellb, Kristi Coec, Joy Hansond, Robert Snydere, Aleda Chenf
a PhD, IMFT, Professor, Dept of Psychology, Cedarville University, Ohio, USA
b PharmD, BCPS, Professor, School of Pharmacy, Cedarville University, Ohio, USA
c MS, MLIS, RN, Professor, Cedarville University School of Nursing, Ohio, USA
d Student, Department of Psychology, Cedarville University, Ohio, USA
e MD, President, HIS Global, Pennsylvania, USA
f PharmD, PhD, Professor, School of Pharmacy, Cedarville University, Ohio, USA
Providing spiritual care to patients can result in improved health outcomes and health-related quality of life. However, healthcare professionals feel largely unprepared to address spiritual health. The objective of this study was to determine the impact of an interprofessional training session on student spiritual health and perceived confidence and competence in sharing their faith with patients. An all-day, interprofessional workshop to assist students in assessing their own spiritual health, identifying opportunities to address patient spiritual health, and sharing their faith ethically was incorporated. Nursing, pharmacy, allied health/kinesiology, psychology, and pre-med students attended and completed assessments related to the student outcomes pre-workshop, post-workshop, and at 3, 6, and 9 months post-workshop. Significant improvements in perceived confidence and competence were documented initially and longitudinally. Baseline student spiritual health was high; only participation in Christian activities significantly improved in the assessment of their spiritual health. Further study is necessary to fully understand the impact of this training on student spiritual health. Nonetheless, incorporation of this training can better prepare students to engage in spiritual care of patients and share their own faith with others ethically as opportunities arise.
Key words: spiritual vital signs, training, healthcare workers.
When experiencing a chronic or acute illness, patients face a variety of concerns that go beyond physical aspects. Providing unidimensional care instead of holistic care leaves an unfulfilled gap for these patients, as spirituality enhances health-related quality of life in chronic disease.1 MacLean et al. surveyed patients in a primary care setting and found that 66% of them thought that their physicians should be aware of their religious or spiritual beliefs.2 In a survey of 54 studies, Best, Butow, & Olver found that a majority of patients express interest in discussing religion and spirituality in medical consultations.3 Patients perceive that spirituality discussions may assist in positive religious-based coping, greater collaboration, and increased faith.4
Although including spiritual care in consultations has been shown to reduce medical costs5, improve quality of life6, and lead to less aggressive care at the end of life,7 many healthcare professionals feel uncomfortable addressing spiritual care directly and refer patients instead to clergy or chaplains.8 This is likely due to factors such as confusion about the differences between spirituality and religion and about how religion is regarded in the healthcare setting.8 In a study of family medicine residents, Saguil, Fitzpatrick, and Clark found that as few as 12% of them have received training in spiritual care and indicated that they would be more likely to provide spiritual care or initiate discussions with further training, particularly if the training provides evidence on the importance of it.9
It may be important that healthcare providers build and cultivate their own spiritual health to address their own challenges (burnout, attrition, etc.), improve resilience, and increase career satisfaction.10 VanderWeele et al. suggest that accessing their own spiritual resources can build resilience in healthcare workers. They also note the reciprocal relationship between providing medical care and accessing spiritual resources—that through providing care, clinicians can better access their spiritual resources.10
Given the lack of training in school and the importance of addressing one’s own spiritual health as well as the patient’s, it is important that health profession schools determine ways to prepare their students for this aspect of practice. Very few approaches exist in the literature that address both personal spiritual health and how to provide patient spiritual care. Thus, the objective of this study was to determine the impact of an interprofessional training session on students’ spiritual vital signs and their perceived confidence and competence in sharing their faith with patients.
This study received Institutional Review Board (IRB) approval from Cedarville University - exempt status.
The Saline Process, which was named so because it relates to the medical IV solution that is often used for patient treatment but also refers to Christians being “salt” and “light”, was offered by IHS Global. It is an educational endeavor to prepare Christian healthcare workers to care for the spiritual needs of their patients while also caring for their physical needs11. The Saline Process also encourages Christians to examine, cultivate, and strengthen their own personal faith journey and is focused on equipping healthcare professionals to share their faith in the healthcare setting while adhering to commonly accepted ethical standards as well as workplace rules and regulations. The training addresses five main questions: “1) Why is faith important in healthcare?; 2) What are the opportunities for and barriers to fulfilling God’s call?; 3) What is my part?; 4) What tools will help me cultivate, sow, and harvest?; and 5) Where do I go from here?”11 The training includes a didactic portion, as well as integrated learning activities (i.e., reflection questions about personal spiritual vital signs, opportunities for sharing faith, etc.) for students or healthcare professionals to complete both individually and in groups over the course of 6–8 hours. Students/healthcare professionals also follow the entire healthcare journey from the beginning of healthcare because of an auto collision until the end of care of a patient as part of the learning experience, with opportunities to practice their patient interactions and learned skills with role play during the training. The IHS curriculum includes instructions on how one of the trainers of the Saline Process training should act as a patient and then allows time for the students in the training to “interact” with the patient. Time also is spent ensuring students understand the ethics of this approach in the midst of workplace rules and regulations as well as respect for patient preferences and values. As part of the training that students received for addressing spirituality in patients, they were instructed to consider their own spiritual vital signs, which include characteristics such as their competence and compassion for patients.11
This Saline Process training was provided at no charge (including the presentation of material, the material, and the facilitation of activities and discussions related to the training) for a group of health profession students at a Christian university to prepare them to provide spiritual care in their future practice as well as address their own spiritual health. All students who attend the university are asked to make a declaration of their Christian faith as part of the admissions process. Similar requirements are present for faculty and staff. Full-time faculty from pharmacy, nursing, kinesiology/allied health, and psychology underwent training in the Saline Process and became certified trainers. These faculty members all had practiced or currently practice in their disciplines. Two cohorts of students completed the Saline Process training in an eight-hour, one-day training period during the 2017–2018 (N=179) and 2018–2019 (N=134) academic years. Students were excused from class to attend the training.
In August 2017, first professional year Doctor of Pharmacy (PharmD) students and sophomore nursing students were required to attend the training session. Students from other health profession majors (allied health/kinesiology, psychology, and pre-medicine) could elect to attend. On the day of the event, students were broken up into groups of 7–8 per table across 4 rooms of faculty trainers. Each table had at least one pharmacy student, one nursing student, and one other health profession student. Rooms held no more than 50 students each to maximize opportunities for student participation in the large group setting.
After reviewing student feedback and discussion amongst trainers and faculty, it was decided to offer the training to students with a higher level of clinical experience in August 2018. Senior nursing students were required to attend. Students from other health profession majors (pharmacy, allied health/kinesiology, psychology, and pre-medicine) could elect to attend. For the second training, the students who attended had not attended the first training. Students were again broken up to allow as much diversity in their majors at each table as possible.
To assess the study objectives, surveys were administered pre-training, immediately after the training and at 3 longitudinal intervals (3, 6, and 9 months) (see Figure 1).
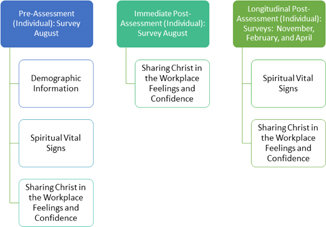
Figure 1. Timing of Assesments
The surveys were modified from ones utilized by IHS Global.11 Demographic information was obtained along with survey information in 3 areas: 1) self-assessment of Spiritual Vital Signs (7 items: 2 items about belief in Christ, 5 items about frequency of faith activities); 2) agreement about the importance of different aspects of biblical witness (5 items: 5-point Likert-type agreement scale, 1=Strongly Disagree, 5=Strongly Agree); and 3) confidence in biblical witness (5 items: 5-point Likert-type confidence scale, 1=Not at all Confident, 5=Extremely Confident). Agreement and confidence questions included the same concepts with differences in whether they were confident in performing the item or agreed with the importance of or preparedness to perform an item.
SPSS v. 25.0 was used to analyze the data. Variables were described using frequencies, medians with an interquartile range (non-parametric data), and means with a standard deviation (parametric data). Changes in Spiritual Vital Signs between the pre-assessment and the first post-assessment were examined using a Wilcoxon test and changes across all assessments with a Friedman’s ANOVA.
As shown in Table 1, demographic data were collected on the cohort. Most students were in pharmacy or nursing, female, sophomores, and had limited patient experience. Only 5 participants (2.9%) were not from the United States.
When comparing the pre-Saline training results to that of 3 months post-training, only question 5 (participation in Christian activities/ ministries) was statistically significantly higher than pre-training assessment in participation in Christian activities/ministries, with students indicating greater frequency of participation (p<0.05, see Table 2). When changes were assessed longitudinally at 3, 6, and 9 months related to Spiritual Vital Signs, only question 5 (How often do you participate in Christian or church-based activities/ministries?) was significant (p=0.008). No statistically significant differences were found for the other survey questions (see Table 2).
A number of changes were statistically significant in the survey items related to the importance of and preparedness for sharing faith in the clinical setting immediately after the training session (see Table 3). Longitudinal changes across all assessments were significant (p<0.001) for all statements measuring level of agreement with the importance of biblical witness, with the exception of two. Both the importance of sharing faith with patients (p=0.146) and the importance of sharing faith with other professionals (p=0.442) did not have a statistically significant change. Longitudinal changes across all assessments were significant (p<0.001) for all statements measuring level of confidence with respect to biblical witness.
This study presents a first step in preparing students to approach spiritual care and provides an assessment of students’ spiritual health as it relates to their confidence in approaching spiritual care in professional practice. Our findings show that students had a midpoint level of confidence and preparedness for having spiritual conversations with patients prior to the Saline Process training with median responses at neutral or below, despite believing in the importance of doing so. We also found that students who attended the Saline Process training reported increased participation in Christian activities/ministries after the training. These findings are of importance because they may indicate that training related to integrating faith in clinical practice encourages students to increase activities that can enhance their own spiritual health.
Assessing a patient’s spiritual need and responding to prompts that a patient may be interested in having a conversation can be challenging for health professional students as well as practicing professionals.8,12,9 Yet, it is important to prepare students to have conversations with patients about spiritual care, as patients with many different chronic diseases indicate spiritual care as an unmet need.13 Failure to address this need can be linked to poorer health outcomes.1,14,15,4 Intentional integration in the curriculum with role models and the opportunity to practice and apply skills in an ethical manner can be an effective tool in meeting this need.12 Indeed, healthcare providers indicate a need for evidence-based training to break barriers in providing spiritual care.13,8,9 This training addressed these key needs by providing an evidence-based approach for spiritual care.
Training for healthcare professionals, and students, also can incorporate how to listen actively and follow the patient’s leading for opportunity identification and provision of ethical spiritual care.12,16 Our training provided interprofessional, faculty role models with practice experience, an opportunity to practice and apply skills with each other and the faculty, and a discussion of how to approach spiritual care legally and ethically. These elements, along with providing training on patient spiritual care, likely resulted in the significant initial and longitudinal improvements of student perceived importance as well as confidence in approaching spiritual care and sharing their own faith. A training for nurses regarding the spiritual care of patients also resulted in similar increases in knowledge and self-perceptions of preparedness.17
Healthcare providers may benefit from attending to their own spiritual health.10 Throughout their careers, healthcare professionals may face burdens and challenges as part of patient care as they help patients navigate through acute and chronic diseases. Spirituality also may be a key component in a healthcare professional’s job satisfaction.18,10
Thus, it may be important to train students in how to best support and share their faith with other healthcare professionals. Further, Cone and Giske interviewed nursing students and faculty and found that their ability to care for their patients spiritually depended on their maturity and especially on how secure they felt in their own faith. As they matured in their faith, they were better able to remain relaxed with their patients when spiritual issues were discussed.12
How do we determine if someone is ready to provide spiritual care? One example of readiness assessment is similar to an APGAR (Appearance, Pulse, Grimace, Activity, and Respiration) score for newborns, wherein a healthcare provider’s spiritual well-being or vitality may be assessed by looking at their circulation (connection to the head and body of Christ), ventilation (prayer), muscle tone (participation in activities and ministry), nutrition (receiving biblical teaching, reading, and study), and reproduction (making of disciples).11 One way to measure these Spiritual Vital Signs is to reflect on each of these areas as an individual and adjust, if needed. Our training provided students with an opportunity for such an assessment as part of active learning during the training sessions. Students in our study were able to gain confidence in providing spiritual care which also significantly increased their involvement in faith-based activities. Given that these students were at the mid-point of their college years and had high baseline scores in their Spiritual Vital Signs, it is not unexpected to see limited improvement with the ceiling effect of a 5-point Likert-type scale. It is our hope that these students have the preparation they need for future practice.
This study was done at a single Christian institution. Thus, it will not be generalizable to all settings. The survey instruments were not validated, although they were modified from previously utilized but not validated surveys from IHS Global. Further, there may be social desirability bias present in this study. Students may choose responses related to their Spiritual Vital Signs to provide spiritual care based on the perceived “correct” choices. We attempted to minimize this by making the surveys voluntary and anonymous. Further, the group was fairly homogenous and had a high interest in spiritual issues. These types of issues have been commonly reported in spirituality training studies.19 Self-assessment also is limited in its scope and applicability19; it would be beneficial to consider a competency-based assessment in the future to substantiate the findings. There also was some attrition in completing the surveys over time, so this may impact findings from the research.
Incorporating a training for future Christian healthcare professionals may result in improved confidence and knowledge in providing patients’ spiritual care. Students’ own Spiritual Vital Signs changed little, but baseline assessments had high scores. Given the generally positive impact of providing spiritual care for patients on health outcomes and quality of life as well as personal spiritual care on resilience, it is hoped that these students are better prepared for future practice.
Future research in Christian institutions should look at a comprehensive curricular approach, where the concepts are reinforced throughout the curriculum and students are given additional opportunities to apply and practice. The impact of using these skills in clinical, experiential settings should also be assessed to determine how the classroom components and practice translate into the workplace. Triangulation of the data with qualitative perspectives may also provide further insight into the development of students.