Figure 1. Project Change Indicators
CASE STUDY
Judith Siambe Opiyoa, Paul Shetler Fastb
a BS in Public Health Nutrition and Dietetics, Program Officer, Center for Peacebuilding and Nationhood (CPN), Kenya Mennonite Church, Kenya
b MPH, MA (International Development), Global Health Coordinator, Mennonite Central Committee, Haiti
Progress on maternal and child health has been slow and uneven in Africa, with widening geographic and socio-economic disparities despite economic growth and continued investments in health systems. In Kenya, modest national-level gains mask wide disparities in progress, with near stagnation among the very poor, those with the least education, and those living in either extremely rural contexts or dense informal urban slums. Progress toward Kenya’s maternal and child health Sustainable Development Goals will depend on finding new ways to work effectively in dense urban slums where poverty and ill-health are increasingly concentrated. Effective approaches require addressing significant knowledge, behavior, and trust gaps, especially with the most vulnerable residents of slum communities like Nairobi’s Mathare. Care groups were designed to address these gaps but have only been effectively tested and scaled in rural and peri-urban environments. The Center for Peacebuilding and Nationhood’s Maternal and Child Health Care Group project supported by Mennonite Central Committee in Mathare, one of the largest informal settlements in Kenya, was one of the first to adapt the Care Group model to an urban slum. Adapting the model was necessary in this challenging context characterized by high population density, crowding, extremely transient and unstable populations, low social trust, lack of traditional social structures, high crime, political disruption, and frequent rapid onset disasters. This study shows the pilot’s success and challenges in adapting care groups to the realities of a dense African urban slum, the innovative strategies the project has used, and the unique benefits of doing this work on a small scale rooted in a local church organization.
Key words: maternal health; child health; social and behavioral change communication; care groups; urban; slum; Kenya
While global maternal and child mortalities have declined significantly in recent years (44% and 42%, respectively, between 1990 and 2015), progress has been extremely uneven, resulting in many countries failing to achieve their Millennium Development Goals. An estimated 99% of all maternal deaths remain concentrated in low- and middle-income countries, particularly in Africa.1 Progress on maternal and child health has been slow and uneven in Africa, with widening geographic and socio-economic disparities, despite economic growth and continued investments in health systems.2 Kenya exemplifies this trend with a recent systematic review showing only modest gains between 1990–2015 in maternal mortality (26%), neonatal mortality (19%), and stillbirths (7%) despite strong economic growth, relative stability, and continued health system investments. However, even these modest national-level gains mask wide disparities in progress with near stagnation among the very poor, those with the least education, and those living in extremely rural contexts and dense informal urban slums.3 As Kenya continues to rapidly urbanize, making progress on maternal and child health, achieving the Sustainable Development Goals (SDGs) will depend on the ability to work effectively in dense urban slums, where poverty and ill-health are increasingly concentrated and older program models have struggled.4,5
Kenya’s recent improvements in maternal and child health (accelerating in the early 2000s) have been driven primarily by expanding access to basic health services; improving HIV testing, control, and treatment; and devolving health services to the local level through the Ministry of Health’s community health strategy.3,6 However, this approach has left significant knowledge and behavior gaps, especially with the poorest and most vulnerable residents of slum communities like Nairobi’s Mathare. These knowledge and behavior gaps have limited many people’s ability to take advantage of available health services and improve their health and wellbeing. These types of gaps are what the Care Group model was designed to efficiently address and why this model was selected by the Kenya Mennonite Church’s Center for Peace and Nationhood (CPN) to address the pressing maternal and child health challenges in Mathare.
The Care Group model is an innovative cascade-style training and behavior change approach for improving maternal and child health in resource constrained settings. It was first designed by World Relief in Mozambique in 1995 as a community-based strategy to facilitate effective and sustained behavior change in a large population at low cost.7 Key elements of the Care Group model include peer-to-peer health promotion, cascade training of contextually adapted maternal and child health curriculum, selection of volunteers by participant mothers, no more than 15 households per volunteer leader, no more than 10 volunteers per promoter (often a specially trained community health worker), at least monthly contact between volunteers and targeted mothers, peer support for improved health practices through group meetings, and regular supervision of the volunteers by more highly trained health promoters.8 Care groups have since been replicated by at least 23 organizations in 27 low- and middle-income countries. These projects were implemented in rural areas except for one case in Cochabamba, Bolivia, where Care Groups were used for promoting behavior change in a peri-urban (non-slum) setting. In Kenya, Care Groups have been implemented by African Medical and Research Foundation (AMREF), HealthRight, Plan International, and JPEGHO, all with large multi-million dollar projects based in rural areas.9 With Kenya’s rapidly urbanizing population, the growth of dense urban slums, and the growing concentration of poverty and maternal and child ill-health in these slums, it is essential to develop effective maternal and child health programming for these environments. CPN’s maternal and child health Care Group project in Mathare, Nairobi, started in 2017, is one of the first published examples of adapting the Care Group model to an urban slum environment.
Mathare is among the largest informal settlements in Nairobi, with a population estimated at between 200,000–500,000 people on just three square kilometers of land, giving it one of the highest population densities in Africa.10,11 Its population is also highly transient, with an estimated 54% of the population having lived in Mathare for less than 10 years and 30% for less than 5 years.12 It is characterized by densely packed and poorly constructed housing units built directly on the ground surface. Mathare is barely penetrated by basic public facilities such as toilets, water, and sewage systems, electricity, police, roads, schools, and hospitals. There is one functional latrine for every 85 households.13 The few resources available are overcrowded by a constantly increasing population. Basic sanitation, hygiene, and health are highly compromised by the crowded environment and lack of basic infrastructure and services. According to the United Nations, children in Nairobi slums are two and half times more likely to die before their fifth birthday than in other areas of Nairobi, and similar statistics exist for most measures of maternal and child health. Malnutrition of mothers and children in these areas is high, as most families live below $1 USD per person per day, and 92% pay over half their income in rent. Acute child malnutrition and stunting rates are estimated at 39% and 47%, respectively, for these neighborhoods, with malnutrition and diarrheal diseases highest among children of young single mothers (aged 15–19).14,15,16 Additionally, as the economic situation has deteriorated in the slums, in order to survive, more women have been forced to choose sex work as a coping strategy, with the percentage of unmarried women who are sexually active increasing 62% from 2000 to 2012, leading to higher rates of HIV, other sexually transmitted diseases, and unplanned pregnancies. Among women with little to no education, the average age of first birth is only 15 years, and many of these women lack the social and family support they would have in rural environments.17 This context is one in which Care Groups appeared to be the most appropriate strategy to help improve health outcomes for vulnerable women and children. While all 14 required criteria8 of the Care Group approach were respected, the uniquely challenging nature of the slum environment, where Care Groups had never been tested before, required significant adaptation.
To successfully adapt Care Groups to the urban slum environment of Mathare, CPN’s team developed strategies for dealing with key differences between Mathare and the more typical rural locations where Care Groups have been successfully implemented. Key challenges of the Mathare context that needed to be overcome in adaptation, included:
As a small, local church-based organization, CPN was also very different from the major international NGO actors who have been the primary implementers of Care Groups. This included a more limited budget of $141,590 over the three-year project cycle, roughly 1/14th of the average budget of Care Group projects reviewed in the published literature.9 This smaller size and local church grounding meant CPN lacked some of the institutional, technical, and administrative resources to facilitate complex monitoring systems, rapid implementation, and scale-up. However, its small size, rootedness in a local church, and having all local staff allowed CPN to be nimble in quickly adapting programming and strategy to meet local realities and more quickly build trust. CPN was supported in this work through a financial grant and technical accompaniment from Mennonite Central Committee (MCC), a US and Canada-based Christian NGO with offices in Nairobi that has been a long-time partner of CPN.
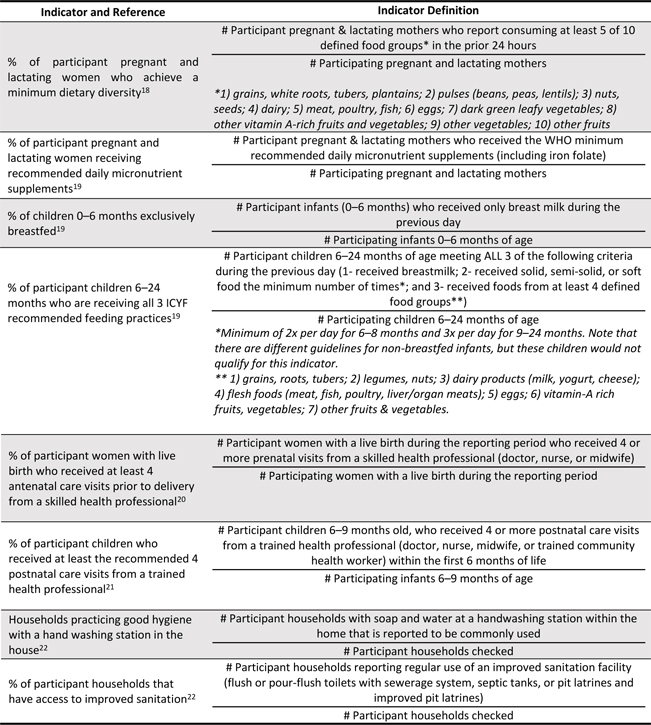
This research study represents a two-year, longitudinal analysis of CPN’s Care Group adaptation pilot in Mathare, Nairobi. At the onset of the project, a transect walk was conducted to map Mathare 3A, 3B, and 3C villages. These three adjoining areas of Mathare were selected because they had the highest levels of maternal and child malnutrition and the lowest rates of antenatal and postnatal care. These areas are considered the most insecure parts of Mathare and, for that reason, many other health projects have abandoned or avoided the area. After this transect walk, a survey was done to gather baseline data against which progress toward the project’s outcomes and indicators could be compared. Due to the small scale and community-led nature of the project, a smaller set of outcome indicators could be tracked than is typical in multimillion-dollar international NGO projects. All indicators were collected and reported twice yearly through household surveys conducted by project staff and trained volunteers. Indicators were selected to provide the most actionable and practical information, be feasible with limited budget and technical staff, and follow internationally recommended indicators whenever possible. A list of the project indicators, indicator definitions, and references in the literature supporting use of these indicators is provided below in Figure 1.
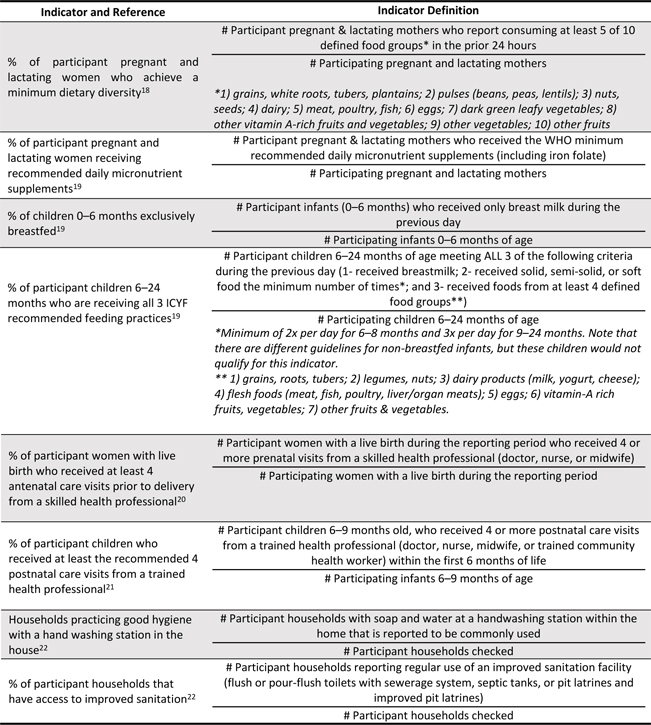
Figure 1. Project Change Indicators
The project was started slowly in order to build trust and test adaptation strategies more easily. It began with a small pilot of the first care groups in one of the three target villages, Mathare 3B. This was done for six months in order to assess the reach, effectiveness, adoption, ability to overcome the unique challenges of working in a slum environment, get new staff up to speed, and ensure the ability to implement and sustain the work successfully. A six-month assessment was done, small adjustments were made, and the project was then scaled up to cover all three Mathare villages (3A, 3B, and 3C).
The project had three full-time staff as supervisors—the coordinator and two project officers. Two of the three full-time staff were nurses, one being a pediatric nurse and the other a nurse midwife. The project coordinator was a public health nutritionist. The project used existing trained community health volunteers as promoters due to their trust and familiarity in the communities and level of health knowledge and experience. The care group volunteers were volunteer women leaders from the neighborhoods. While traditional care groups begin with a complete community census followed by grouping households geographically under community volunteers to ensure saturation coverage, this was not feasible in the Mathare context. The transient nature of urban slums and the lack of trust meant that conducting an accurate census was neither feasible (due to low trust and suspicion of political or criminal motives) nor helpful (since people change household locations frequently). Instead, CPN took advantage of its experienced and trusted local promoters to build up care groups and household groups organically from existing networks. Women were also given the option to stay in the same household group even if they moved geographically within Mathare, allowing for more continuity and low dropout rates (less than 10%). While these adaptations are more complicated than the neat geographic boundaries and 100% saturation coverage of the traditional Care Group methodology, the adaptations were necessary within the context. The promoters organized the household women into groups of 10 and the neighbor women elected their care group volunteers. The care group volunteers were then organized into groups of 10 to form the care groups.
Context specific behavior change communication curriculum and visual flipcharts were then designed and rolled out. The curriculum was adapted from Food for the Hungry’s 2013 curriculum from Ethiopia, focused around four core modules: 1) orientation, maternal nutrition, and breastfeeding; 2) growth monitoring, complementary foods, and micronutrients; 3) care of mothers and newborns during pregnancy and postpartum; and 4) water, sanitation, hygiene, and management of diarrhea. Messages were communicated in a cascade approach where the project coordinator and supervisor trained promoters, who then trained care group volunteers in the care groups, who then taught the direct participants in the neighbor women groups and through home visits. Feedback on the curriculum and rollout of each module as well as basic project monitoring data were relayed back up the cascade through simple monthly reporting forms that captured participant demographics, indicator and output data, participant feedback, challenges being faced, and ideas for improvement. These forms were completed by care group volunteers and shared with promoters who then analyzed and compiled a report to share with their supervisors. Both project supervisors visit each care group at least twice per month, and each promoter visits each neighbor women group at least twice per month for supportive supervision. The project currently reaches 1,950 households, organized into 195 neighbor women groups, supported by 12 promoters.
The success of the project can be measured quantitatively against the tracked indicators and qualitatively in its ability to be accepted by the community, adapted to meet the felt needs of participants, and developed a self-sustaining momentum and sense of buy-in that can support the initiative’s long-term prospects. The chart below (Figure 2) shows twice-yearly progress on tracked indicators with green highlighted rows showing indicators with statistically significant progress in a positive (desired) direction, not highlighted rows showing no significant change, and red highlighted rows showing statistically significant change in a negative (undesired) direction. Since all variables were binary, statistical significance was measured at 24 months using a chi-square test with p-values of less than 0.05 (significant) and 0.01 (highly significant).
Five of eight indicators show highly significant (p<0.01) positive change (desired direction). These included maternal dietary diversity, exclusive breastfeeding, recommended child feeding practices, hygiene and hand washing, and access to improved sanitation (Figure 3). Two indicators (antenatal and postnatal care visits) show no significant change and one indicator (receiving appropriate supplements) showed highly significant negative change (non-desired direction). These unchanged and negatively changed indicators are shown in Figure 4.
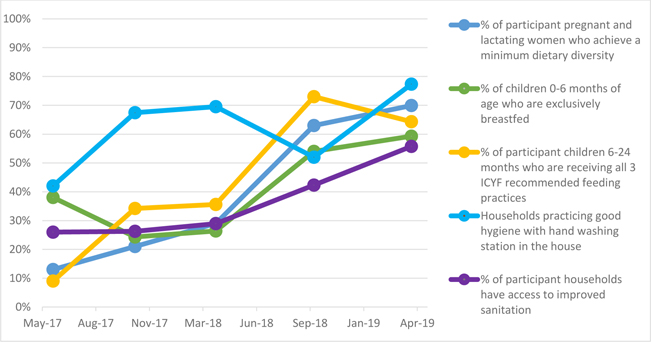
Figure 3. Indicators Showing Positive Statistically Significant Change
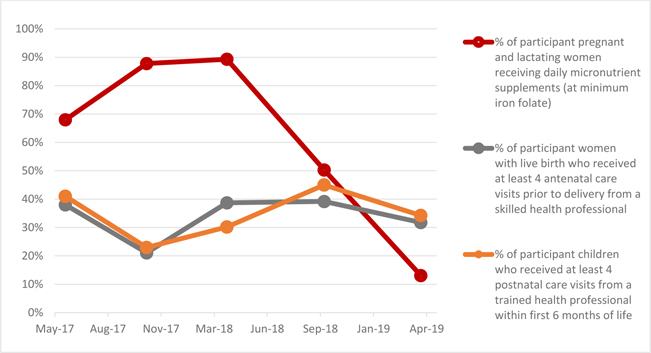
Figure 4. Indicators Showing no Change or Negative Statistically Significant Change
With five of eight indicators showing significant positive change and only one showing significant negative change in such a difficult environment, CPN’s pilot adaptation of the Care Group model to Mathare can be considered successful. Despite the many challenges of operating in this context, the project was readily accepted by participants and the wider community and women were able to make significant behavior change in the areas where they have more direct control. Success in community acceptance was driven by actively involving the local community (through promoters, care group volunteers, and neighbor women) as key actors in the project from the very beginning, through implementation, monitoring, evaluation, and refinement of the approach. Sharing the data from the community with CPN staff and then back to the community was an inspiration to community actors when they could see that their efforts were transforming people’s lives. Being a faith-based organization was an added advantage for gaining rapid acceptance and credibility by the community and local authorities. As a small local organization based in a local church meant that community members, staff, volunteers, participants, and local authorities were less likely to think of the project as a source of personal financial gain or possible extortion, compared with projects implemented by large governmental organizations or international NGOs.
However, the project had significant contextually-driven challenges that it was not able to overcome, which stalled progress on the three project change indicators that are most dependent on interaction with and service availability from the healthcare system (which is largely outside the project’s scope of household behavior change). The three stalled indicators (minimum antenatal care visits, minimum postnatal care visits, and receiving appropriate supplements) struggled because the project depended on (and did not replicate) the public health facilities and services available. However, these services are vastly under-resourced with basic staffing (health care providers) and resources like iron and folic acid supplements. Mathare was also chronically underserved and under-resourced, resulting in overcrowding of the existing facilities and long costly wait times and reduced quality of care. This makes it even more challenging for women to attend care visits instead of pursuing income generation.
Other contextual challenges faced by the project included issues of space, time, transience, and crime. The settlement areas of Mathare 3A, 3B, and 3C are so tightly clustered together that even finding a safe and free open space where women could meet was difficult. For groups, women had to squeeze in the narrow public aisles between their houses (generally less than three feet wide), meaning they were forced to sit in a line rather than a circle and discuss even delicate matters in relatively public spaces. Time was another major constraint for participant women. This was especially true for those who depend on casual day labor and micro-commerce to support their families. With razor thin economic margins, women found it difficult to lose productive work time in meetings or waiting for care. The project sought to maximize the little time available to communicate key information during lessons. This meant being extremely focused in what information was conveyed and doing so quickly and efficiently. The economic vulnerability of the women also meant that once organized into groups, one of their top priorities was to improve their economic wellbeing. These groups were supported in forming micro savings programs and, in some cases, even started shared microbusinesses like beadwork. The pilot was also challenged by the extreme transience of many participants. This made goals like 100% saturation or all women staying in the program throughout their pregnancy and lactation difficult to achieve. Many of the project participants were not able to stay in the same housing units throughout the project. They were constantly on the move, both voluntarily as they searched for more stability and economic opportunity and involuntarily as the result of disasters like fire, forced evacuations, political violence, conflict, and socio-political intolerance. Crime is also frequent in these communities, especially petty thievery, which meant many families struggled to establish handwashing stations as the units were frequently stolen if not brought indoors.
The results of this study support the broader literature on Care Groups. The Care Group approach was designed primarily to improve health knowledge and behaviors at the household and community levels and has been repeatedly demonstrated to be successful in doing that.8,9 This pilot showed similar results with highly significant and positive change in all the indicators over which households had primary control (maternal dietary diversity, exclusive breastfeeding, recommended child feeding practices, hygiene and hand washing, and access to improved sanitation). The three indicators with no significant or negative change (antenatal care visits, postnatal care visits, and receiving appropriate supplements) all depend on government services over which the project and the households have little to no control. During the project, these services were frequently disrupted by strikes, political crisis, and stockouts of essential supplies. These results further support the literature on Care Groups, which has shown that progress on maternal and child health often faces hard limits by factors outside of household and community levels of control and, therefore, difficult for Care Groups to impact as significantly as hoped.9
The CPN-MCC pilot project demonstrated that an adapted Care Group model can have significant impacts on key indicators of maternal, newborn, and child health in the urban slum environment of Mathare, Nairobi, Kenya. However, the significant struggles in improving indicators dependent on access to government health services (antenatal care, postnatal care, and supplements) is a reminder that household-level behavior change may not be enough by itself to fully achieve the SDGs in maternal and child health in these types of contexts.
The limitations of this study, in interpreting and extrapolating the findings, include the lack of a control group, relatively small sample sizes in the early phases of the project, the lack of time and scope sufficient to see impact on ultimate indicators like maternal and child mortality, and the inability to control for other factors and trends outside of the project’s scope. These limitations are primarily the result of this being a small-scale locally led project, with all data being collected first and foremost for use within the project and for the benefit of the direct participants in improving the quality of programming. To fully understand the potential of Care Groups and for it to be adapted to dense urban slums across Africa, further research is required. However, this pilot project has demonstrated that Care Groups can be successfully adapted to this type of context and, at least in this case, show significant results on critical behavior change indicators with a very limited budget, small scale local implementation by a faith-based partner, and in a relatively short period of time. This work has been deeply integrated into the already existing community health systems that the government has put in place in Mathare and works to support those systems and priorities. However, this approach leaves the project’s success somewhat dependent on the quality and availability of those government services.
This pilot supports the literature that care groups can be a highly effective component to fast-tracking achievement of the SDGs in maternal and child health, both in Kenya and beyond. The experience of CPN and MCC in Mathare has demonstrated that this model can be successfully adapted to an urban slum context in Africa, where this type of work is urgently needed.