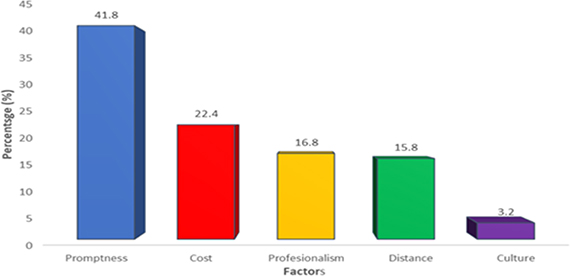
Figure 1. Self-reported factors influencing choice of healthcare
ORIGINAL ARTICLE
Paul West Okojiea, Richard Laneb
a MPH Student, Liberty University, United States of America
b MD, MPH, Professor, Department of Public and Community Health; Program Director, Master of Public Health program, Liberty University, United States of America
Introduction: Health care resources are disproportionately distributed between urban and rural areas in many developing countries, including Nigeria. Barriers to health care like cultural beliefs, poor education, and financial constraints make many rural dwellers seek other options of health care available to them. This paper aimed to determine the sociodemographic factors that influence health-seeking practices in a rural community setting.
Methods: A sample of 380 rural community dwellers in Southern Nigeria was recruited in a cross-sectional study. An interviewer-administered questionnaire was used to collect socio-demographic, healthcare access, and utilization data. Data were analyzed with SPSS version 25.0 software. A chi-square test was used to find the association between sociodemographic characteristics and their health-seeking practices.
Results: Equal proportions (43.4%, 42.9%) of the respondents fell within the younger age categories of 10–29 and 30–49 years. Self-reported factors influencing the choice of health care were: promptness of care (41.8%), cost (22.4%), professionalism (16.8%), distance (15.8%), and cultural belief (3.2%). The patent medicine store was the most utilized source of health care (42.1%), and 36.8% of respondents sought health care in the hospital. The hospital was utilized by 41.8% of respondents with secondary education, 34.9% with tertiary education, 31.7% with primary education, and 26.1% with no formal education. Females tended to seek health care from hospitals (40.2%) and patent medicine store (43.7%) compared to males (33.3% and 41.0%, respectively). There was a statistically significant association between education and health care options utilized (P<0.05).
Conclusion: This study draws attention to the suboptimal utilization of standard health care in a rural community setting mainly due to perceived influences of promptness of health care service (41.8%) and cost (22.4%). It revealed that rural dwellers mainly seek healthcare from patent medicine stores. The health authorities should, therefore, prioritize the eradication of delays at the point of care and expand financial access to health care. These would enable rural dwellers to optimize the minimum standard of health care available within their various communities.
Key words: health-seeking behavior, rural, Nigeria, primary health care
Primary health care (PHC) aims to bring health care as close as possible to where people live and work.1,2 To bridge the gap in health service infrastructure and ease inequitable access to health care by the vast majority, the World Health Organization (WHO) launched the health for all strategy.3 However, after four decades since the Ama Atta declaration, many developing countries have yet to fully operationalize PHC to the level of their sociopolitical and economic development.4,5 Health indices continue to worsen in the affected countries, particularly among the most at-risk groups in the population—women, children, and the elderly.6,7 Consequently, attaining a level of health that will facilitate social and economic productivity has been elusive for many individuals, families, and communities in these countries.
Distributive equity in the allocation of health resources has been hard to realize by many developing countries.8 In many cases, healthcare resources are disproportionately distributed between urban and rural areas.9,10 According to the National Demographic and Health Survey (NDHS), about 64% of Nigeria’s population live in rural areas while many have little or no access to quality healthcare.11,12 Despite the contribution of rural dwellers to food production and preservation of culture, their quality of life is poorer than that of their urban counterparts.13 To correct this social injustice, Nigeria adopted a national health policy that is based on the principle of PHC.14 Unfortunately, the country appears to have made unimpressive gains due to faulty implementation framework, resource deficit, and lack of political will.15,16
In communities where the minimum standard health facility is present, barriers to health care access such as culture, education level, geographical factors, and poor healthcare financing have been identified.17,18 Nigeria is yet to effectively implement universal healthcare coverage, 70% of healthcare spending in the country is out-of-pocket, and rural dwellers are unable to afford exorbitant fees charged in public and private health facilities.19 A sizeable proportion of the Nigerian population, the majority of whom live in rural communities, are yet to attain a level of education required to make them appreciate the benefits of utilizing available health resources like health centers and immunization services. Data from the 2013 NDHS indicate that literacy is generally higher in urban areas compared to rural areas. While more than 7 in 10 urban women (77%) are literate, less than 4 in 10 rural women (36%) are literate. It further showed that literacy levels decline with age, from 66% among women in the age range of 15–19 to 36% among women in the age range of 45–49.20 This, among other identified factors, affect health-seeking behavior and decision-making concerning suitable healthcare options.17-19 Rural dwellers have been reported to combine Traditional African Medicine (TAM) with standard care or fail to utilize health facilities in their domain due to a perceived clash of Western medicine with their cultural beliefs. Similarly, the use of Patent Medicine Stores (PMS, commonly called a “chemist” by a majority of Nigerians) is rampant in most rural Nigerian communities.21 There are premises mandated by regulatory bodies such as the Pharmaceutical Council of Nigeria (PCN) to sell patent medicine or over the counter drugs (OTC) that are considered safe for unsupervised public use as long as they are sold in their original manufacturer packages. Common OTCs include pain-relieving tablets, antimalarials, and cough syrups. PMS is not permitted to sell and dispense prescription drugs such as antibiotics and steroids. Also, most PMS sell household products such as toilet soap, body creams, and canned foods depending on consumer demand.21
The health-seeking practices of a community influence the utilization of available health resources. A study conducted in Wakiso District, Uganda identified regular stock-out of drugs, high cost of services, and long distance to health facilities as factors affecting the health-seeking practices of a community.22 Findings from a study of the effects of access to primary health care services on the health-seeking behavior of Nigerians showed a spectrum of health care options in the community. Over 50% of the respondents sought health care at the health centers, 121 (62.7%) PMS, 87 (45%) medicine vendors, 100 (51.8%) private clinics, 56 (29%) prayer houses, and 118 (61.1%) traditional healers. The researchers identified accessibility to health-care services as the most common reason for the preferred choice of visit among 79.8% of the study participants.23 The study concluded that limited access and delivery of poor-quality health service at the primary health care level accounted for Nigerians seeking non-standard health care.
This study identified the prevailing health-seeking practices of a rural community and the factors responsible for the phenomenon. This information will be useful in developing behavior change strategies to promote better health awareness in the community and enhance health facility utilization. Identification of options of healthcare available in the community will aid public health authorities to engage practitioners to train them and correct practices inimical to health. Therefore, this paper aimed to determine the sociodemographic factors associated with health-seeking practices in a rural community setting in Nigeria.
A cross-sectional study was conducted over six months from June to November 2017 in Utese, a rural community in Ovia North East Local Government Area of Edo State, Nigeria. Utese has an estimated population of 1,320, and the people are mostly peasant farmers and small-scale traders. Some socioeconomic infrastructure available in the community includes a palace led by a village headman, market, primary/secondary school, and a primary health center.
Residents who had lived in the community for a minimum of six months before the study were included, while those who did not consent to participate in the study were excluded. The Cochrane formula for calculating sample size in a cross-sectional study was used to estimate a total sample size of 345. Three hundred and eighty (380) respondents who consented to participate in the study were selected through a systematic sampling technique. A random selection of the palace was carried out, consequently; every third house was also selected and respondents who met the inclusion criteria were interviewed.
A structured, interviewer-administered questionnaire was used to collect data on socio-demographic and preferred healthcare choice and health-seeking behaviors of the respondents. Data were sorted for completeness, coded, screened, and entered in the SPSS version 25.0 software for statistical analysis. Univariate and bivariate analyses were conducted for appropriate variables. Sociodemographic data were presented with summary statistics as means and proportions. A chi-square test was used to find the association between respondents’ sociodemographic characteristics and options for health care. Statistical significance was set at p<0.05.
Approval for the survey was granted by the Department of Community Medicine, Igbinedion University, Okada, Nigeria. Permission was sought from the Local Government Chairman, the head of the council of chiefs of Utese. The verbal consent of respondents was sought before the administration of the questionnaires.
Respondents were assured of their right to participate and withdraw from the study at will. Confidentiality of data was ensured by deidentifying respondents during data entry with the use of serial coding only. All data were safely stored in a secured and password-protected computer accessible only to the researcher.
Respondents within the younger age categories of 10–29 years (43.4%) and 30–49 years (42.9%), made up 86.3% of the study sample. Of the 380 participants, 51.1% of them were female and 48.9% males. Fifty-eight percent of respondents were married while 41.6% were unmarried. Fifty-one percent of respondents attained secondary education while 31.6% attained primary education. Seventy-two percent of them had lived in the community between 1–29 years and 25.3% earned a monthly income of N 26,000–50,000 ($70–$140) (Table 1).
Forty percent of respondents aged 10–29 years chose hospitals for health-care compared to those aged 30–49 (33.7%). Of respondents aged 10–29 years, 44.8% chose patent medicine stores compared to those aged 30–49 (43.6). Of those aged 70–89 years, 37.5% chose traditional medicine. A chi-square of independence showed that there was no significant association between age of respondents and choice of healthcare, X2 (12, N =380) = 19.5, p = .07 (Table 2).
One-third of male respondents used hospitals, while 40.2% of females used hospitals. Men chose a patent medicine store (33.3%) and self-care options (5.4%) for healthcare compared to women (40.2%, 5.2%). A chi-square of independence showed that there was no significant association between age of respondents and choice of healthcare, X2 (4, N =380) = 6.26, p = .17 (Table 2).
Respondents with a primary (31.7%), secondary (41.8%), and tertiary (34.9%) level of education used hospitals for healthcare. Traditional healers (26.1%) and self-care (13.0%) were reported among those without basic education. Of respondents with primary school education, 15.1% used traditional healers. A chi-square of independence showed that there was a significant association between the education of respondents and choice of healthcare, X2 (12, N =380) = 22.19, p = .03 (Table 2).
Forty percent of respondents who had lived in the community for 3 to 6 decades used hospitals, while 35.2% of them used patent medicine stores and faith healing. Of respondents who had lived in the community for less than 3 decades, 12% used traditional healthcare, while 36.9% of them used hospitals. A chi-square of independence showed that there was a significant association between the amount of time lived in the community by the respondents and their choice of healthcare, X2 (8, N =380) = 16.06, p = .04 (Table 2).
| Healthcare Option Utilized (n=380) | ||||||
|---|---|---|---|---|---|---|
| Traditional | Hospital | PMS* | Faith Healer | Self-Care | P | |
| Age (Yrs) | ||||||
| 10–29 | 18 (10.9) | 66 (40.0) | 74 (44.8) | 3 (1.8) | 4 (2.4) | 0.06 |
| 30–49 | 22 (13.5) | 55 (33.7) | 71 (43.6) | 5 (3.1) | 10 (6.1) | |
| 50–69 | 8 (18.2) | 17 (38.6) | 13 (29.5) | 0 (0.0) | 6 (13.6) | |
| 70–89 | 3 (37.5) | 2 (25.0) | 2 (25.0) | 0 (0.0 | 1 (12.5) | |
| Sex | ||||||
| Male | 21 (11.3) | 62 (33.3) | 90 (48.4) | 3 (1.6) | 10 (5.4) | 0.17 |
| Female | 30 (15.5) | 78 (40.2) | 70 (36.1) | 5 (2.6) | 11 (5.2) | |
| Marital Status | ||||||
| Married | 35 (15.8) | 74 (33.3) | 91 (41.0) | 6 (2.7) | 16 (6.8) | 0.10 |
| Unmarried | 16 (10.1) | 66 (41.8) | 69 (43.7) | 2 (1.3) | 5 (3.2) | |
| Education | ||||||
| None | 6 (26.1) | 6 (26.1) | 7 (3.4) | 0 (0.0) | 4 (13.0) | 0.02** |
| Primary | 19 (15.1) | 38 (31.7) | 49 (40.8) | 4 (3.3) | 10 (8.3) | |
| Secondary | 20 (10.3) | 81 (41.8) | 86 (44.3) | 3 (1.5) | 4 (2.1) | |
| Tertiary | 6 (14.0) | 15 (34.9 | 18 (41.9) | 1 (2.1) | 3 (7.0) | |
| Income/month (N=) (N= 360=$1) | ||||||
| 1,000–25,000 | 36 (12.7) | 100 (35.2) | 128 (45.1) | 6 (21.0) | 13 (4.6) | 0.36 |
| 26,000–50,000 | 15 (15.6) | 40 (41.7) | 32 (33.3) | 2 (2.1) | 7 (7.3) | |
| Duration of residence (Yrs) | ||||||
| 1–-29 | 33 (12.0) | 101 (36.9) | 123 (44.9) | 5 (1.8) | 12 (4.4) | 0.04** |
| 30–59 | 12 (13.6) | 36 (40.9) | 31 (35.2) | 3 (35.2) | 6 (5.7) | |
| 60–89 | 6 (33.3) | 3 (16.7) | 6 (33.3) | 0 (0.0) | 3 (16.7) | |
Notes: *=Patent Medicine Store **=statistically significant
The reasons for the healthcare options utilized included promptness (41.8%), the cost (22.4%), distance from dwelling place (15.8%), professionalism displayed (16.8%), and culture considerations (3.2%). (Figure 1)
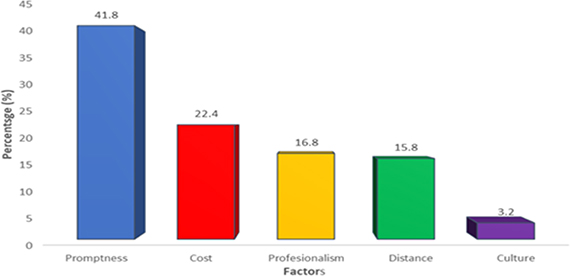
Figure 1. Self-reported factors influencing choice of healthcare
The patent medicine store was the most utilized source of health care (42.1%). One hundred and forty respondents (36.8%) sought health care in hospitals, while 13.4% used traditional healers. (Figure 2)
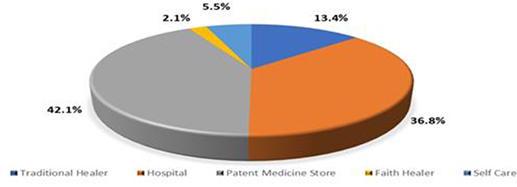
Figure 2. Proportion of respondents by self-reported rural healthcare option utilized
The demographic profile of the participants in this study reflects Nigeria’s young population with over 80% of the study subjects belonging to the age brackets of 10–29 and 30–49 years. According to the data, the younger-aged respondents appeared to use hospitals more than the middle-aged and elderly respondents. In most rural communities, the elderly people are the custodians of traditions and the perceived health benefits of traditional African healing.24 This may explain the observed high user rate of traditional healers among the elderly compared to the younger respondents in the study sample.
This study revealed a gender difference in the health-seeking practices of the community. It showed that compared to 40% of women, only one-third of men used hospitals in the community. This relatively poor use of hospitals by the male respondents is not unexpected since beliefs about masculinity and manhood, which are deeply rooted in most African cultures, influence health-seeking behavior in many rural communities. The social system in many African communities projects men as strong, dominant, virile, and invulnerable compared to women.25 This, unfortunately, translates into an exhibition of unhealthy attitudes such as fewer encounters with the health system, poor treatment adherence, and a delay or refusal to seek prompt healthcare among men.26,27 On the other hand, the higher proportion of women seeking hospital care in this study corroborates the finding of previous studies which showed a higher utilization of health services and better health-seeking behavior among women compared to men.28,29 This may not be unconnected with the physiological role of women in childbearing and related childcare functions like infant/child nutrition and immunization which necessitates women to frequent healthcare facilities.
In this study, a significant association was found between education and health-seeking practices. A higher proportion of respondents with secondary and tertiary education were more likely to report the use of hospital care compared to those with primary or no education. This finding is in keeping with the well-documented role of education as a determinant of health.30,31,32 Education has been linked to the social and psychological factors that affect health. Previous studies have shown that people make better health choices when they are educated.31,32,33 Education is known to be associated with improved health knowledge and better employment opportunities which create economic empowerment and lead to financial access to quality healthcare/services. In a rural setting, this can facilitate uptake of preventive and treatment services and reduce the overall disease burden in the community.
As the most populous country on the African continent with a substantial number of rural dwellers, the demand for healthcare in rural Nigeria is satisfied through various health service outlets.34 This study revealed that the participants (42.0%) majorly sought healthcare from patent medicine stores. This proportion is lower than that of a previous study in a rural Nigerian community which reported a 62.7% utilization rate of PMS.22
PMS are perceived to be a more accessible and affordable source of healthcare service in many relatively poor communities in the country. This perception may account for why PMS is mostly preferred among the spectrum of healthcare options in the community. Besides, 42% of the respondents identified promptness of service to have the most influence on their choice of healthcare. This may further buttress the finding of a higher PMS utilization rate. Operators of PMS are individuals who are well known to the community, and this relationship potentially helps to overcome the barriers to prompt health service delivery such as a delay due to distance from the source of care and extensive pretreatment documentation. This observation, however, raises a concern about the standard of care administered by PMS practitioners in rural areas and its implication for the overall health of the community. Also, it provides an opportunity for health administrators to investigate the factors accounting for poor utilization of standard medical care despite the presence of a primary healthcare center in the community.
Closely tied to the perceived influence of promptness of health service delivery is cost. In this study, the cost of healthcare service was the second most reported factor influencing the respondents’ choice of health care. A previous study has identified finance to play an important role in ensuring healthcare access in rural Africa.35 Most rural dwellers are poor and can barely afford the cost of hospital care which has been on the increase in recent times, and this may explain their choice to utilize alternative sources of healthcare such as traditional healers or faith healers. This can potentially lead to the exclusion of a large segment of the population from accessing standard health care, thus making them prone to complications of substandard treatment procedures from poorly trained local care providers. The resulting poor health will lead to low economic productivity, further deepen poverty, and increase proneness to more disease.36
As shown in the study, there was a significant association between the length of stay in the community and health-seeking practices. It is known that time is crucial to learning, hence long-term residents are naturally expected to be more aware of the available healthcare options in a community. It is, however, unclear the extent to which such awareness due to length of stay in a community can influence health-seeking behavior. Therefore, this finding of a significant association between length of stay in the community and health-seeking practices may be artifactual.
This study may be limited by self-reporting bias. The fact that this study was done in one small rural community may make its findings less generalizable. Besides, the non-inclusion of a qualitative component, like a focus group, may have restricted the scope of analysis of factors influencing the choice of healthcare in the community. Further community-based studies should incorporate qualitative tools to explore the potential role of community gatekeepers and ward health development committees in championing positive health-seeking practices. Rural-based health service research with a focus on quality management will address the community’s perception of cost and timeliness of health service delivery. Besides, a follow-up study should address the nature and type of illnesses which may have influenced the health-seeking in the study participants. The authors acknowledge that this study does not provide information on the proportion of faith-related or tradition-related problems compared to modern healthcare-related problems which may have explained the patterns of health care utilization in this study.
This study draws attention to the suboptimal utilization of standard health care in a rural community setting mainly due to perceived influences of cost and promptness of health care service. It revealed that rural dwellers mainly seek health care in patent medicine stores. It further showed education and duration of stay in a community as significant determinants of health care options. The health authorities should, therefore, prioritize the eradication of delays at the point of care and expand financial access to health care. These would enable rural dwellers to optimize the minimum standard of health care available within their various communities.