
Figure 1
ORIGINAL ARTICLE
Caleb Flinta, Vijay Anand Ismavelb, and Ann Miriamc
a JD, MBA, Wharton School of Business, The University of Pennsylvania, Philadelphia, PA, USA
b MBBS, MS(General Surgery), MCh(Pediatric Surgery), Senior Administrative Officer, Makunda Christian Leprosy and General Hospital, Bazaricherra, Assam, India
c MBBS, MD, Consultant Anesthesiologist, Makunda Christian Leprosy and General Hospital, Bazaricherra, Assam, India
Background: Mission hospitals in low-resource regions of the world face significant challenges in providing high-quality, accessible care to patients. External funding is limited and can fluctuate significantly from year to year. Additionally, attracting and retaining well-qualified healthcare professionals for more than short stints can seem almost impossible. Located in a remote region in Northeast India, the Makunda Christian Leprosy & General Hospital has developed a model over the past 25 years that has enabled it to sustainably expand access to high-quality care for the region’s poor, which we evaluate in this paper.
Methods: We combine an external assessment by a research team at the Wharton School of Business with internal insights from two leaders at Makunda Hospital to evaluate the Makunda Model. The external assessment included 31 in-depth, on-site interviews of patients, employees, and competitor hospital administrators; physical observation of Makunda’s facilities and operational practices; and an analysis of years of financial documents and hospital statistics.
Results: We studied the impact of the Makunda Model on volumes, efficiency, quality, and community impact. In 2018-19, Makunda Hospital provided 109,549 outpatient visits, 14,731 hospital admissions, 6,588 surgeries (2550 major), and 5,871 baby deliveries in a 162-bed facility with a bed occupancy rate of 88%. The hospital operates with an annual budget of $2.7M ($1 = INR 75.70) and receives only 2.5% of its operating revenue from external sources. The hospital has developed a strong reputation in the community and beyond for providing excellent maternal care and catering to the poor.
Discussion: The hospital’s business model revolves around two key business strategies: (a) poor-centric strategies and (b) thoughtful cost management. Innovative poor-centric strategies include “ability-to-pay”-based pricing, equal services for all (in contrast to a freemium model), hyper-tailored charity (using the “shared meals” and “vital assets” tests), and community engagement. Thoughtful cost management is accomplished by “revised gold standard” treatment protocols and recruitment and retention of an efficient workforce.
Conclusion: We conclude that Makunda Hospital’s unique combination of poor-centric strategies and thoughtful cost management have enabled it to achieve the volumes necessary to sustainably improve access to care for the poor in Northeast India.
Key words: poor-centric strategies, equal services, charity, Christian mission hospitals, Makunda model
The Makunda Christian Leprosy & General Hospital,1 founded in 1950 by Baptist Mid-Mission USA, is located in a remote region in Northeast India at the border of three neighboring states: Assam, Tripura, and Mizoram (see Figure 1). Originally a leprosy colony on 1,000 acres of land, the hospital became a general hospital from the late 1950s until the early 1980s, when the expatriate staff running it were asked to leave India. Consequently, the hospital fell into a state of disuse until 1992 when it became a member of the Emmanuel Health Association (EHA), an association of 20 independent hospitals in India.2
In October 1992, two of the authors, Drs Vijay Anand Ismavel and Ann Miriam from the South Indian state of Tamil Nadu, visited the hospital and were impressed by the area’s needs. They were motivated by a search for a location that provided the highest potential for transformational impact, as determined by the population that they could serve divided by the number of other similar care providers. Makunda was situated in a place that was moderately populated with no other comparable hospital within 100 km. It also had a large campus that could be used to provide other services in the future. Since EHA felt that it could not safely assume responsibility for a hospital in such a remote location, the founding doctors gave a career-long commitment to serve there for 30 years. The early days were difficult, but they persevered in spite of the challenges.3
To cover the full time period they planned to stay at Makunda Hospital, Drs Vijay and Ann developed a 30-year strategic plan with three key phases. Phase I was aimed at stability: resolving tensions with local community members and generating enough revenue to cover costs. Phase II focused on local expansion, including building a secondary school, nursing school, and branch hospital to serve the community. Finally, Phase III centered on distant impact, including developing and sharing best practices with organizations in other low-resource settings. This period also included a new community college, a nature club, and a larger emphasis on agriculture.
Today, 25 years into its strategic plan, Makunda Hospital has completed two phases and is well into its third. In the 2018-2019 fiscal year, the hospital provided care for 109,509 outpatients, had 14,731 inpatient admissions, performed 6,588 surgeries (2,550 major), and conducted 5,871 deliveries. It also opened another branch in Tripura, a neighboring state, that served 7,838 of these patients in 2018-19. Makunda Hospital provides its services at very low prices and provides 15% of its income as charity to poor patients.
Furthermore, Makunda Hospital has created various educational and agricultural businesses. It runs a K-12 school system with over 1,000 students, a nursing college with 61 students, and a nurse assistant training program with 43 students. Most of the nursing college and nurse assistant program students stay in dormitories provided by Makunda Hospital. On the agricultural side, Makunda owns a farm that generates food for its school hostels for most of the year, and it owns several fisheries and a piggery. Finally, Makunda Hospital recently designated a wildlife area within its boundaries and created the “Makunda Nature Club” to document and publish biodiversity records.4 All of these activities are performed to further Makunda Hospital’s mission to provide Christian service to the people of Northeast India regardless of their background (see Appendix I for the hospital’s mission statement).
The goal of our observational study was to assess the impact of the Makunda Model on access to quality healthcare within Northeast India and to identify the underlying drivers for the hospital’s financial sustainability and success. A team of students from the Wharton School of Business conducted the external research assisted by a faculty member and generated an initial report about the model.5 The team focused its research on how Makunda Hospital utilizes poor-centric strategies and thoughtful cost management to provide high-quality care to the poor.
Our observational study is primarily descriptive and relies on a mixed methods research design. We relied on three approaches to gather and triangulate the necessary data: (1) in-depth interviews, (2) facility observations, and (3) document analysis. The interviews provided qualitative insight about the impact of Makunda Hospital and the drivers of its impact, verified through facility observations and by reviewing and analyzing hospital statistical and financial documents. Makunda Hospital's Management Committee and Research Committee provided permission for the study and provided access to the hospital's financial and statistical information. Statistical data for other EHA hospitals were taken from publicly available reports. IRB approval was not deemed necessary for the study.
A total of 31 in-depth interviews were conducted by the Wharton research team of (a) Makunda Hospital employees, (b) hospital patients and community members, and (c) competitor hospital administrators and staff, as summarized in Table 1.
First, confidential interviews were conducted by a Wharton research team member with 16 Makunda Hospital employees in a broad range of roles, including managerial, clinical, teaching, and technical positions (see Appendix II for details). At the beginning of each interview, interviewees were informed of the purpose of the study and that any information they disclosed may be shared in an anonymized format with hospital management or in a published report, but that no statements would be personally attributed to any specific individuals without their permission. Interviews focused on the strengths, weaknesses, changes, differentiators, and impact of Makunda Hospital (see Appendix III for the full list of survey questions used). After the unique drivers behind the Makunda Model were identified (i.e., poor-centric strategies and thoughtful cost management), additional questions were used to probe deeper. Interview notes were coded by these drivers and reviewed by the other members of the Wharton research team.
In addition, a Wharton research team member visited five local communities representing a broad cross-section of the hospital’s patients to understand how patients and their families view Makunda Hospital. A total of 7 in-depth interviews were conducted, most with the assistance of a translator. The five communities included the following groups: (1) tea garden laborers, among the poorest people in Indian society and who usually live in crowded primitive huts and earn around INR 100 ($1.42 USD) per day; (2) members of the Brahmin community, who tend to occupy leadership positions and live in larger homes with electricity; (3) members of the Vaishya community, which include skilled laborers who live in humble homes on their own land; (4) members of the tribal community, who cultivate rice for work and live in more isolated communities; and (5) Muslim families, who make up about a third of Makunda Hospital’s patients.
Finally, hospital administrators and staff from three competitive hospitals in Northeast India, including two government hospitals and another mission hospital (also a member of EHA), were interviewed. Questions focused on the services and value proposition of those hospitals versus Makunda Hospital. The following individuals were interviewed in-depth, with additional physicians and staff providing comments throughout the tour of the facilities:
To understand Makunda Hospital’s model, an extensive tour of the facilities was conducted, and the outpatient experience was followed from check-in to the waiting area to the physician consultation to the pharmacy. Significant time was spent observing patients and operational practices in each of these areas. Then the lab testing rooms, operating rooms, and inpatient facilities — which include 162 beds across the female ward, male ward, maternal ward, pediatric ward, postnatal ward, high dependency unit, and NICU — were toured. Finally, other facilities surrounding Makunda Hospital, including the Makunda primary and secondary schools, nursing and nursing assistant schools, grain farms and fisheries, physician and staff dormitories, and wildlife preservation area were visited. For purposes of comparison, the facilities of both government hospitals and the other mission hospital were also toured.
Makunda Hospital provided financial and statistical documents for review. This included over 10 years of historical revenue and cost data and detailed patient volume statistics. Makunda Hospital’s annual report and Emmanuel Hospital Association’s annual reports (obtained from their website) were reviewed and various financial analyses were conducted to understand Makunda’s model and how it compares to other hospitals both in the United States and India. Finally, the patient complaint log and statistical data on hospital complications and mortalities were reviewed.
Based on these in-depth interviews, facility observations, and detailed document analysis, the Makunda Model and its impact on the local community were evaluated.
The impact assessment of Makunda Hospital’s volume, efficiency, quality, and overall community impact are presented below:
In the 2018-2019 fiscal year, Makunda Hospital completed 109,549 outpatient visits (a 7.7% compounded annual growth rate (CAGR) from 2014-19); 14,731 inpatient admissions (6.0% CAGR); 6,588 surgeries (10.2% CAGR); and 5,871 deliveries (5.1% CAGR). Figure 2 shows Makunda Hospital’s growth in deliveries and surgeries for the period from 2007 to 2019.
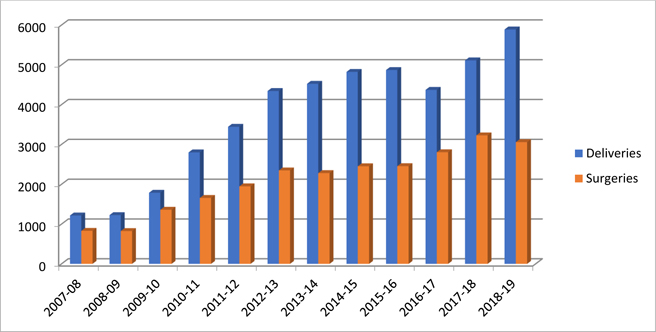
Figure 2. Makunda Hospital’s Growth in Deliveries and Surgeries, 2007-2019
To put these numbers in context, we looked at the Emmanuel Hospital Association6 (the largest Christian non-profit healthcare provider in India with 20 hospitals and 40+ community-based projects), where the average hospital had 45,825 outpatient visits; 5,034 inpatient admissions; 1,542 major surgeries; and 1,245 deliveries. Of the 19 EHA hospitals reported, Makunda Hospital was the largest by number of outpatients, deliveries, and surgeries, and second largest by number of inpatients and beds. Furthermore, many of the other EHA hospitals are facing declining patient volume, as opposed to Makunda, which has seen consistent CAGR growth over the past several years.7 Although there are many external factors which affect statistics among different EHA hospitals (such as competition from nearby hospitals or lower population densities), it is notable that Makunda has grown to become one of the highest-volume EHA hospitals despite starting off as a completely closed-down hospital 25 years ago.
For an additional point of comparison, the average hospital in the U.S. has 7,745 discharges per year, with urban hospitals hitting 11,295 discharges per year on average, and rural hospitals reaching 2,467 discharges per year on average.8 Furthermore, U.S. hospitals tend to see about twice as many outpatients as inpatients per year, far below Makunda Hospital’s numbers.9 Overall, Makunda Hospital has achieved very high patient volume, especially considering its location in a remote area of India, as seen in Figure 3, by expanding access to quality healthcare services.
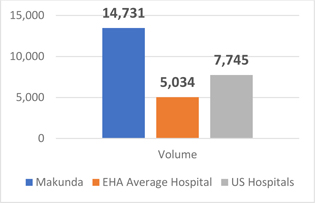
Figure 3. Comparison of Average Hospital Inpatient Volumes
In achieving these volumes, Makunda Hospital operates on a total budget of $2.7M USD (for 2018-19), which includes the total costs for the hospital, educational, and agricultural portions of its operations. The income from the hospital alone is $2.2M and accounts for 83.9% of income. The non-hospital activities run at a loss and are subsidized by hospital income. Furthermore, Makunda Hospital has run efficiently enough to reinvest nearly 6.5% of its annual revenue in new buildings and equipment (in 2018-19) and to write off 15% of its bills to charity. For the fiscal year 2018-19, the average outpatient cost was only $11.56 USD (INR 875), and the average inpatient cost was only $68.03 USD (INR 5150), figures that were substantiated by examining detailed accounting and financial documents. These numbers represent very efficient costs per patient treated, particularly given that less than 2.5% of operating revenue comes from external sources.10
Makunda Hospital is well-known for its high-quality services, particularly in maternal care. To make our assessment of quality, we examined the hospital’s certification, key performance metrics, and qualitative interview responses.
First, Makunda Hospital has achieved entry-level certification for safety and quality from the National Accreditation Board for Hospitals and Healthcare Providers (NABH).11 Such a certification requires passing an extensive audit process, creating a detailed quality assurance process that includes continuous tracking of certain metrics, and meeting stringent standards for the treatment and disposal of medical waste products.
Second, Makunda Hospital tracks favorably on key metrics for hospital quality, including overall inpatient mortality and maternal mortality rates. In 2018, the overall mortality rate in the hospital was 2.0%, down from 2.4% in 2016. The proportion of maternal deaths among mothers who delivered in Makunda similarly declined from 0.5% in 2016 to 0.1% in 2018. Considering that many community members come to Makunda Hospital only for their most complicated births (as noted by those we interviewed), this is particularly indicative of its standards of quality. The hospital has been part of a private-public partnership with National Health Mission Assam for maternal and child health services since 2008 and is recognized as a referral center for high-risk obstetrics patients in the district. Makunda’s impact on local measures of health is also noticeable. For example, as shown below in Table 2, the MMR and IMR rates for the region dropped significantly in the district of Karimganj during the years (2009 to 2013) in which Makunda Hospital sharply increased its number of deliveries (as captured above in Figure 2).12
| Year | 2009-10 | 2010-11 | 2012-13 |
|---|---|---|---|
| MMR per 100,000 live births | 474 | 342 | 281 |
| IMR per 1,000 live births | 87 | 69 | 69 |
During interviews, we found near-universal respect for Makunda Hospital among both competitive hospital administrators and community members. One government hospital administrator indicated his hospital loses “many, many patients” to Makunda Hospital despite the fact that Makunda Hospital charges for its services (as opposed to government hospitals, which are essentially free) and despite the fact that it is located hours away. Though he had not visited Makunda Hospital himself, he said, “We hear from patients that the services are much better there; people tell us that it is well-managed, patient satisfaction is high, and it has good cleanliness.” Another government administrator said that Makunda Hospital was well respected by their staff of doctors, and many of this hospital’s patients know it for its strong maternal services and travel hours to go there instead for baby deliveries. One hospital staff member at the Burrows Memorial Christian Hospital stated that Makunda is “probably the best-run mission hospital in India” and added that many healthcare professionals like to start their careers there because of the great training it provides.
When local community members were visited, one previous patient asserted that Makunda Hospital is the “best hospital in Assam” and “we know that they will take care of us.” Similar confirmations of the community’s trust in Makunda Hospital were made in each of the five communities who were visited. In the tea garden community, one mother said that she brought her dying son to Makunda Hospital at the urging of friends despite believing it was too late. Her positive experience with her son’s recovery led her to bring back her three other children over the years and to strongly recommend the hospital to any of her friends who need services.
Makunda Hospital is unique from many private hospitals in India in that it was founded specifically with the intent to help the poor, and its management team has proactively worked to ensure that all hospital policies and decisions are carefully designed to benefit them. In 2018-2019, 15% of its patients received charity for the services it provides; in many cases, these patients would otherwise not have received treatment at all and would have died or lived with great pain. Over time, Makunda has built a reputation for low baseline prices and charity for those who cannot afford even these prices, and more generally for taking care of anyone who comes to its doors.
While Makunda Hospital has had a substantial impact on healthcare in the local community, interviews revealed that its impact extends far beyond that to the community at large, including a K-12 program started in 2004 that educates more than 1000 students each year. In addition to its K-12 education program, Makunda operates a nursing assistant program started in 2015 and a nursing school program started in 2006 to train local community members in preparation for working at Makunda Hospital and other locations. Both of these training programs are subsidized by the hospital so that poor communities can access these services. In addition to education, Makunda provides direct employment to hundreds of people, with cascading benefits on the local economy. Some people we interviewed described the transformation they have seen in the local marketplace over the past few decades as more people with more income have stayed in the area because of the employment and educational opportunities. The government has also recognized the value of Makunda as a service provider for the local community, bestowing it with the Chief Ministers Certificate of Commendation in 2015, and has invested money in local infrastructure and provided support for new hospital construction projects.
Analyzing data from interviews, documents, and facility observations to understand how Makunda Hospital achieves such levels of impact, we found that Makunda Hospital’s business model revolves around two key business practices: (1) poor-centric strategies, and (2) thoughtful cost management. These business practices enable Makunda Hospital to operate a business model of generating higher total earnings by providing very high volumes of very low-margin services. This approach permits Makunda to achieve economies of scale and lower prices, drawing in more price-sensitive patients, which in turn creates more scale and enables them to further lower prices — creating a virtuous cycle. Makunda Hospital has also been able to attract talented young professionals seeking good training opportunities at a high-volume facility. These business practices — poor-centric strategies and focused cost management — are the keys to this virtuous high-volume, low-margin, strategic advantage.
Makunda Hospital employs a range of innovative poor-centric strategies that have enabled it to drive high patient volume in a low-resource setting which drive demand. These include (a) an ability-to-pay based pricing approach, (b) equal services for all, (c) hyper-tailored charity, and (d) addressing cultural barriers to usage through community engagement.
(a) Ability-to-Pay Based Pricing Approach.
Traditionally, hospitals decide on a set of services to offer and adopt “costing” methods to fix prices. Instead, Makunda asked the question, “What can the poor afford to pay?” and then figured out how to provide services that fit within that price point. This was based on community engagement in the early years; for example, the cost of an outpatient consultation was fixed as the cost of having a village haircut. This decision — to start with consumer’s ability to pay — drove all the other decisions regarding costs. Many hospital patients are already hard pressed to pay for a car ride to the hospital, which often costs more than the actual hospital services. The decision to make the hospital’s price points more accessible was the difference between touching only a wealthier subset of the population and reaching nearly the full local population — with important implications for a high-volume, low-margin strategy. Costly services such as treatment in an intensive care unit (ICU), which can quickly impoverish a poor family, are substantially lowered at Makunda Hospital through internal cross-subsidies from other departments, where costs are easily affordable and large volumes generate greater departmental profits. To illustrate, ICU care at Makunda (including ventilation and all procedures but excluding drugs) is charged at INR 650 ($8.60 USD) per day. This is cross-subsidized by income from other departments such as ultrasound, which performed 16,854 higher-margin ultrasound scans in 2018-19.
(b) Equal Services for All.
Another key decision made early on was to provide equal services to all patients regardless of wealth. Many mission-driven hospitals utilize what amounts to a freemium-like model, in which wealthy individuals pay much more for much better services in order to subsidize services to the poor.13 In these models, the wealthy are placed in a separate, shorter queue; receive private rooms; and have a private consultation with a physician of their choice. In contrast, the poor are placed in the longer queue and in general inpatient wards.
The problem with the freemium-like model is that the wealthy expect better services because they know they are paying more and, thus, demand more attention from physicians and staff. In addition, to keep their business, hospital administrators must cater to the needs of wealthier patients by providing what they want, when they want it. Over time, the organization and processes of the hospital become increasingly oriented towards providing services for the wealthy at the expense of the poor — often unintentionally. As this occurs, the poor feel more and more out of place in the hospital and come to see themselves as second-class citizens, so they come less and less often and refer their family and friends less and less often. At the end of the day, this reduces volumes, which reduces scale and increases costs, which requires higher pricing to compensate — creating a vicious cycle.
In contrast, Makunda Hospital has held to its philosophy of providing equal services to all patients, regardless of wealth. The hospital is unique in that it has no private wards, only general wards with reasonable privacy. According to Makunda administrators and employees, this practice is probably the most obvious evidence of equal treatment for the poor when they come to the hospital. This has served to bolster Makunda Hospital’s brand as a place for the poor to go, which drives volumes and revenue up while simultaneously upholding the ideals that led the founding doctors to reopen the hospital in the first place.
(c) Hyper-Tailored Charity.
In fulfilling its mandate to help the poor, Makunda Hospital — like many other mission hospitals — frequently provides services to poor patients for free. Doing so exposes mission hospitals to both type I and type II errors; that is, they may fail to provide aid to those who truly need it, or they may provide aid to those who do not actually need it and lose the corresponding revenue they could have earned to support their hospital.
What makes Makunda Hospital unique is the hyper-tailored methods it uses to both identify those who truly need charity and to provide it to them in the most effective manner. Historically, Makunda Hospital has identified the poor primarily through a set of behavioral observations, and more recently, it has experimented with more formalized diagnostic tools. Two notable examples of behavioral observations — the “shared meals test” and “vital assets test” — merit specific mention. These observational criteria to diagnose financial vulnerability and the risk of destitution are currently being studied and validated by the hospital.
First, in the shared meals test, physicians and nurses (who spend the most time with patients) are instructed to pay attention to the meal habits of family members and friends who accompany a patient at the hospital. If family members and friends frequently skip meals or share a single meal among multiple people, they are identified for charity. This is based on the fact that poor people are willing to go through suffering to get treatment, a behavior that is difficult for wealthy patients to fake.
Second, in the vital assets test, Makunda employees pay attention to how patients act with regards to their medical bills. The poorest of patients will frequently ask how much an additional service will cost and may try to limit their stay in the hospital when they feel they have exhausted their budget even when a doctor recommends that they stay longer. Interestingly, the founding doctors found that the poorest patients are actually much less likely to ask for charity than the moderately well-off patients, who are more likely to try to negotiate on hospital bills to get them reduced even though they can afford to pay. In contrast, the poor typically go to great lengths to pay a bill, including selling so-called “vital assets” that they need for basic living (such as their home) or to maintain their livelihood (such as a work animal or farming equipment). One technique Makunda employees use is to ask how a patient will pay for a planned or billed medical expense. If the patient says they have the money, will be able to borrow the money, or will sell some non-essential items, they are allowed to do so. However, if they mention sale of a “vital asset” that is specially mentioned on a list created by Makunda, they receive charity. Furthermore, if Makunda Hospital finds out after the fact that a patient has sold a “vital asset” (often a distress sale at low value), it goes out into the community and repurchases the asset on behalf of the patient.
If a patient says that they will need to sell a vital asset in order to pay for services, they are asked how much they could pay if they do not sell the vital asset. They are then asked to pay that amount, and the rest is written off as charity. Many poor people have a strong sense of dignity and often ask for the pending amount to be kept as “due” rather than ask for charity. One practice Makunda engages in is to write off all “due” amounts at the end of the financial year.
Another way Makunda Hospital provides charity in a targeted way is to write off large medical expenses related to unexpected complications. Since complications happen so infrequently, writing them off is a relatively small cost for the hospital to incur when spread across many procedures, while not doing so would impose a huge financial burden on a single individual. In effect, Makunda Hospital is providing a form of informal insurance to make healthcare more accessible to the poor.
From a business perspective, Makunda Hospital’s unique focus on identifying and providing tailored charity enables it to retain revenues from those who can afford to pay — essentially operating as a form of efficient price discrimination — and drives patient volume by reinforcing Makunda Hospital’s brand as a hospital for the poor, by retaining patients, and by encouraging referrals.
(d) Removing Cultural Barriers Through Community Engagement.
During the early years of Makunda Hospital, it sought to expand its labor and delivery services but initially faced slow growth. At the time in Northeast India, most villages had an informally designated woman to help with childbirth within that village. This midwife also helped with household work like cooking and taking care of the children when the mother had her delivery, thus, ensuring the least disruption to the family. This practice was so convenient that villagers were willing to forget about the occasional maternal death, saying that it was inevitable. Based on local infant and maternal mortality rates, the founding doctors knew that many mothers and babies were dying during childbirth, but when they asked the de facto village midwife in each of the villages if they had seen any deaths, each of them indicated that they had not. However, by digging deeper, the doctors realized that the village midwives were witnessing significant infant and maternal mortality but were afraid to admit it and were secretly terrified of complicated deliveries — such as malpresentation, hemorrhage, and eclampsia — but did not know what to do about them because their communities looked to them as the experts.
In response, Makunda Hospital began to encourage village midwives to send only their most complicated cases to the hospital. When a village midwife brought such a complicated patient to the hospital, doctors at the hospital explained to the family that the mother’s life had been saved because of the timely referral by the midwife. When referred patients found that they had a good experience at the hospital, they referred friends and relatives for their deliveries too. The midwives became trusted community members in the eyes of both the villagers and the hospital. By seeking to understand the barriers to usage and building community partnerships, Makunda saw large growth in the number of deliveries performed, helping it to achieve its strong reputation within maternal care as a hospital for everyone, especially the poor.
In summary, each of these four poor-centric strategies — an ability-to-pay-based pricing approach, equal services for all, hyper-tailored charity, and addressing cultural barriers to use through community engagement — play into the success of Makunda’s high-volume, low-margin approach.
Given its commitment to providing care to the poor, Makunda Hospital has by necessity always been intensely focused on cost management — the “supply side” of their operating model. To succeed in providing low-price services, it has primarily reduced costs to its patients through two innovative methods: (a) implementing a “revised gold standard” of care that reduces unnecessary testing and procedures for patients, and (b) recruiting and retaining individuals who are willing to accept lower salaries and heavier work obligations because of the training opportunities it provides or their commitment to Makunda Hospital’s mission. These themes emerged through triangulating comments from Makunda employees with financial data on workforce and procedure costs.
(a) “Revised Gold Standard.”
Medical students are often taught the “gold standard” approach to medicine: a broad set of tests and procedures that should be done to maximize diagnostic accuracy and patient health in an ideal world. Unfortunately, physicians in low-resource settings typically do not have the luxury of running all of the tests and procedures outlined under the “gold standard” of care for two reasons: first, their facility may lack the necessary medical equipment; and second, the patients they treat may simply not be able to afford such full-scale services.
To deal with these realities, Makunda Hospital has developed a set of “revised gold standards” to provide services that are affordable to its patients. These standards serve to impact both how physicians make clinical assessments and what lab tests, procedures, and drugs they recommend to patients. Doctors at Makunda think about the cost versus benefit of a test before asking for it. The same process is used for prescription of medicine — a patient is more likely to comply long-term with a set of drugs that the patient can afford.
As another example, Makunda performs choledochoduodenostomies as an alternative to endoscopic retrograde cholangiopancreatography (ERCP) in patients with calculi in the common bile duct. Drs Vijay and Ann have published several articles on interventions that are as safe and effective or nearly as safe and effective as much more expensive alternatives commonly used today during their postgraduate studies.14,15,16
Makunda Hospital’s “revised gold standard” approach has enabled it to lower the cost of providing health care services so it can in turn lower prices, which drives greater volume.
(b) Recruitment and Retention of Efficient Labor.
In addition to practicing its “revised gold standard” practices, Makunda Hospital has lowered costs for patients by recruiting and retaining individuals who are willing to accept lower salaries and heavier work obligations because of the training opportunities it provides and their commitment to Makunda Hospital’s Christian mission.
Government hospitals tend to pay physicians and nurses nearly twice as much as Makunda Hospital, and many government physicians work in their own private practice in the evening after leaving the government hospital, further boosting their salaries.17 Employees at Makunda Hospital noted that the hospital also gets much more leverage from employees by asking them to multitask throughout the day and work longer hours to meet the high patient load. A typical nurse at Makunda Hospital works eight hours a day, six days a week, but may also voluntarily work overtime during a particularly busy shift transition. Because salaries make up the largest expense category for most hospitals, being able to reduce that cost translates to significant savings for patients and contributes to the hospital’s low-price approach.
Despite the heavy obligations and lower salary, many employees choose to work at Makunda Hospital either because of the training it provides or their commitment to the mission of Makunda Hospital. Because Makunda has a nursing school on site, skilled physicians, and high patient volume, many aspiring nurses come to Makunda Hospital to get large-volume, high-quality experience before moving on to other hospitals. Even more striking, however, is the strong commitment to Makunda’s mission that starts with the founding doctors and extends to employees in both the hospital and the school system. Most of the people who were interviewed cited their commitment to Christian service and Makunda’s focus on the poor as the driving force in their decision to work at Makunda Hospital. Furthermore, despite the heavy obligations, these employees tend to find great satisfaction in their work; or in the words of one supervisor, they leave their shift “tired, but happy and content,” knowing their work is full of purpose.
Makunda Hospital leaders constantly reinforce the culture of commitment by challenging the predominantly Christian staff — all Makunda’s professional staff are Christians — to live by Biblical principles of service (such as “walking the second mile”). The hospital’s efforts to develop the school system have also helped to retain young professionals with families who might have left sooner but now have viable local educational opportunities available for their children.
There are some factors that may limit the transferability of this model to other hospitals in low-resource settings:
Despite these potential limitations, we believe that mission hospitals can successfully adopt elements of the model — including some of the poor-centric strategies and thoughtful cost management techniques — to expand access to much-needed healthcare services throughout the world.
Many of the principles identified above can be used by mission-focused healthcare providers in low-resources settings around the world. For example, hospitals can drive volume by utilizing poor-centric strategies such as setting prices according to ability to pay, creating equal services for all patients, tailoring charity according to observable indicators of true need, and engaging with the community to overcome cultural barriers to usage. They can also reduce costs (thus enhancing their ability to lower prices and virtuously drive up volumes even further) by creating customized “revised gold standards” and decrease labor costs by providing a work environment conducive to training and a strong commitment to service.
Factors such as low population density and the presence of closely situated competition may limit the transferability of this model. The absence of a variation in income levels of patients will also not permit internal cross-subsidy. Additional research and study are needed to understand how much these factors play a role in Makunda Hospital’s success and how well the model can be transferred to other settings.
Nonetheless, we believe that this study illuminates several extremely promising and innovative approaches to providing high-quality, accessible care in low-resource settings that can be applied elsewhere. We invite others to engage in additional research and study to substantiate and refine the claims made in this paper. Indeed, some of the general principles warrant further evaluation in the context of discussions about healthcare costs around the world. In conclusion, we believe that the “Makunda Model” developed by Drs Vijay and Ann offers encouragement for those seeking to provide high-quality, accessible healthcare in low-resource settings across the world.
Makunda Christian Leprosy & General Hospital aims to provide high quality medical care at costs that are affordable to the people of North-East India through development of appropriate health care models
The hospital also aims to provide comprehensive services to all, irrespective of caste, religion, race or sex, with the assets at its disposal and through collaboration with other like-minded agencies to improve the social, economic and spiritual lives of our target people.
The hospital further aims to create and sustain a pool of trained manpower and inculcate in them the values of Christian service as exemplified by the life of our Lord Jesus Christ.
| Serial Number | Designation |
| 1 | CEO / Pediatric Surgeon |
| 2 | Anesthesiologist, Correspondent (Training Programs) |
| 3 | Medical Superintendent, Physician |
| 4 | Deputy Medical Superintendent, Pediatrician |
| 5 | Psychiatrist |
| 6 | Resident – MD (Global Health) from Netherlands |
| 7 | Vice-Principal – Nursing School |
| 8 | Principal – Community College |
| 9 | Nursing Superintendent |
| 10 | Nursing School Tutor |
| 11 | Principal – Higher Secondary School |
| 12 | School Teacher |
| 13 | School Teacher |
| 14 | Civil Engineer |
| 15 | Biodiversity Project Staff (ex-student of School) |
| 16 | Hospital Manager |
Initial List
Additional Probing Questions