
Figure 1: Locally made PPE Prototype
CASE STUDIES
Gnanaraj Jesudian a, Kevin Gnanaraj b, Biju Islaryc, Botoho Sumid, George Mathewe
a MS (Gen), MCh (Urology), FICS, FIAGES, FARSI, International Federation of Rural Surgeons, Adjunct Professor (biomedical engineering), Karunya University, and Director Medical Services, SEESHA, Coimbatore, Tamil Nadu, India
c MS (Gen), Crofts Memorial Christian Hospital, Assam
d MBBS, DNB (Rural Surgery), Medzhiphema Community Health Center, Nagaland
e MS, MD, Shanthi Bhavan Medical Center, Jharkhand
The COVID-19 pandemic with the suddenly announced lockdown in India caused great stress to already resource-constrained rural mission hospitals. Frugal innovations helped some of the mission hospitals cope with the lockdown and resume regular work. Personal Protective Equipment was made locally and staff were trained to take care of the infected patients. Cell phones and the zoom app helped them with communications. The Gas Insufflation Less Laparoscopic surgical technique helped them perform safe surgeries and allow quicker turnover of patients. The innovative Laptop Cystoscope helped in follow up treatment of patients treated earlier by specialists and for emergency treatment. Empowering local mission hospital doctors and modern communication methods helped these hospitals maintain services during the pandemic.
Key words: COVID-19, GILLS, Laptop Cystoscope, Personal Protective Equipment
The Christian Coalition for Heath reported that currently there are 70,000 inpatient beds in the Catholic and Protestant mission hospitals in India.1 These facilities are the major non-profit providers of health care for the rural population. In India, the pandemic has lowered the utilization of services ranging from 30% to 69%.2 Since the beginning of 2020, the number of deaths due to COVID-19 is only a tiny portion of the total number of deaths due to any cause.2 Most of the hospitals under stress are in remote locations, do not have significant fund reserves, and need to send employees out for supplies.3 We describe some of the frugal innovations that helped the rural mission hospitals survive during the pandemic.
Innovations were collected from three rural hospitals where the Association of Rural Surgeons of India have training programs for rural surgeons. The Shanthi Bhavan Medical Center [SBMC] is situated about 150 kilometres from the nearest town, Ranchi, from where they need to get supplies. It is the only hospital with facilities for Intensive Care in the entire district of Simdega, which is the most rural district of Jharkhand. The Crofts Memorial Christian Hospital with 60 beds is at Tukrajhar in Assam, near India’s border with Bhutan. The third hospital is in Nagaland, in a small village called Medzhiphema, and has 20 beds.
The innovations involved making local Personal Protective Equipment [PPE] rather than depending on donations or purchases, conducting consultations using zoom meeting software, performing minor surgical procedures under supervision using the zoom meeting software, limiting surgeries to the more relevant and less expensive, and caring with compassion, a hall mark of mission hospital care.
The following are the innovative ways that were followed at these mission hospitals.
SBMC first made a prototype from the locally available materials as shown in Figure 1.

Figure 1: Locally made PPE Prototype
After using it a few times, the hospital then produced them in bulk as shown in Figure 2.

Figure 2: Production of local PPE
Figure 3 shows a training session. Training started many days before the first suspected COVID-19 patient came to the hospital.
Further innovations were needed for examining and treating patients. To start with, they did not have a non-touch thermometer. Hence, a 2-meter long handle with a tray held the usual thermometer which the patient took and used to measure temperature. Figure 4 shows the equipment for examining the patient and Figure 5 for admitting the patients.

Figure 4: Local patient examination set

Figure 5: Apparatus for admitting the patients
Once the hospital was identified as a COVID care hospital, it became difficult to separate the regular patients from those suspected of having COVID-19 infections. Another problem was that many consultants from other hospitals and medical colleges visited the hospital to help. Many patients had Double “J” stents [DJ stents] placed after Urology treatment. They were told to report for stent removals within 3 months of placement. With the lockdown extending for more than 3 months, these patients needed consultations and advice.
The zoom application was used for consultations. The zoom meeting links were sent to the patients, their relatives, the hospital staff, and the doctors involved along with the reports of the patients. Written advice was sent following the zoom consultation. The feedback from the patients was that zoom consultations were much better than telephone calls that had been used earlier.
The camera of the cell phone was used to share the screen using the zoom software so that the specialist from a remote location could guide the local surgeon during procedures like DJ stent removals and DJ stent placements. Figure 6 shows the picture of one surgery in progress.
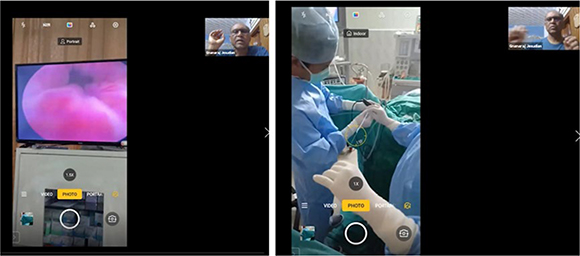
Figure 6: Zoom supervised DJ stenting
Laparoscopic surgery carries the highest risk of aerosols due to pneumoperitoneum with CO2.4 Also, SARS CoV 2 is detected in peritoneal fluid in concentrations higher than in the respiratory tract.5 The use of GILLS is recognized by the WHO Compendium of innovative health technologies in low- and middle-income countries and makes laparoscopic surgeries possible under spinal anaesthesia.6 In rural areas, the technique offers advantages such as shorter hospital stay, lower chances of contamination, and fewer persons required in the operating room.7 It is recommended by the Association of Rural Surgeons of India, the International Federation of Rural Surgeons, and the Association of Surgeons of India.8 Figure 7 shows the GILLS device in use.

Figure 7: The Stan Laparoscopy Position-er TM in use
The Crofts Memorial Christian Hospital started GILLS surgeries with zoom supervision after isolating pre-operative patients who had no symptoms of COVID-19 or any contact with COVID-19 positive areas for 7 days.
Two of the hospitals were able to use the low-cost Laptop Cystoscope shown in Figure 8 to remove and insert DJ stents using the zoom meeting software for supervision and guidance during the procedure.
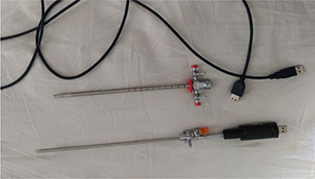
Figure 8: The Laptop Cystoscope
This is an innovative device that has a camera instead of a telescope and connects to the Laptop computer. Prior DJ stenting and ureterorenoscopy are innovative methods for treating renal and ureteric stones in rural areas.9 The use of the zoom app helped with supervision of the surgery from a remote location. The cell phone camera’s pictures could be shared through zoom using the screen share facility and remote guidance in pointing out the orifice and monitoring the progress was possible.
The time available due to the lockdown was used to work on research projects that would be useful in the future.
Currently available PPE were not comfortable to wear and health care workers were eager to take them off after their use. Skin injuries and complications were common. In one of the studies, they found that “Soaked skin combined with pressure increased the friction coefficient between the PPE and skin, and when masks and goggles were removed quickly, skin tears happened.”10 The authors designed a prototype shown in Figure 9 that makes PPE comfortable to wear.
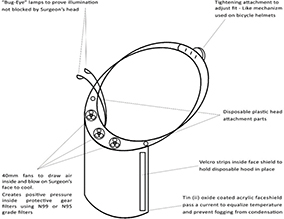
Figure 9: Prototype for comfortable PPE
It has cooled, filtered air pumped in so that there is some positive pressure for safety and cool air inside for comfort. The Peltier thermo-cooler effect could be used for cooling, and a special coating and passing electric current could prevent fogging. Special powerful LED lights could help too.
The authors are also working on a remotely controlled Robotic Unit that has facilities for measuring pulse rate, oxygen saturation, and blood pressure in addition to transmitting voice and pictures. Height, weight, and Body Mass Index, blood sugar, and haemoglobin are possible additional non-invasive measurements we are considering for future addition.11 We are also working on a remote controlled robotic unit with a camera that could allow a closer look at areas of interest. Later, these arms could be used for holding ultrasound probes, camera, or instrument while helping with surgical procedures from a remote location. Figure 10 shows the base model on which these additions are planned.

Figure 10: Remote controlled Robotic assistant
Caring for the sick has long been considered a hallmark of Christianity. Christian health care workers cite biblical references of the call to medical missions as an example of God’s unconditional love (Matthew 10:8; Luke 10:8–9, 25–34). Although Christians have been involved in medical missions throughout history, participation in short-term medical missions (STMMs) has grown dramatically in the past few years.12
The pandemic highlights the problem with the STMM when the local doctors are not able to do the work of the visiting faculty. However, empowering local surgeons helps them to continue to work to the best of their ability.13
Thanks to the training by the Association of Rural Surgeons of India, the local surgeons were able to carry on the surgeries with GILLS and Laptop Cystoscope. The visitors to the mission hospital were able to support the hospitals by donating to the hospital which paid for the PPE and the staff’s salaries. The staff also contributed to mitigate the crisis by offering to take payment only for their needs during the pandemic rather than taking their full salaries.
The staff also participated in the zoom lectures on GILLS so that the surgeons in other low and middle-income countries (LMICs) in Africa could benefit from their experience. The patients appreciated the efforts of the staff.
The pandemic forced the local LMIC hospitals to be more autonomous and to problem solve rather than relying on help from outside. The rural surgery associations played an important part in supporting these hospitals with necessary guidance and innovations.