
Figure 1. Swollen and painful left side of the neck of patient.
CASE REPORT
Ferdy Royland Marpaunga, Aryati b, Sidarti Soehitac
a Department of Clinical Pathology, Faculty of Medicine, Univeritas Airlangga Dr.Soetomo Hospital, Surabaya, Indonesia
Acute suppurative thyroiditis (AST) is a rare clinical entity that must be treated immediately because of its morbidity, especially swelling in the thyroid area accompanied by fever. AST is often preceded by infection at another site; therefore, it is important to identify the source. A 40-year-old woman came to the Dr. Soetomo General Hospital complaining of pain and swelling in the neck, difficulty swallowing, and fever. The patient suffered from chronic kidney disease. One week before, she had an infected arteriovenous hemodialysis shunt. Laboratory results showed an increased fT4 (3.5 ug/dL) and a decreased TSH (0.015 uIU/mL), leukocytosis, and a raised C reactive protein (CRP). Thyroid ultrasound showed an abscess involving the entire left thyroid. Thyroid fine needle biopsy showed AST. Culture of the pus grew Staphylococcus aureus. The thyroid tests supported the diagnosis of AST with hyperthyroidism; immediate treatment was indicated. Three weeks after treatment, the patient was euthyroid and still had drainage of the wound. The AST was considered to be secondary to the hemodialysis AV shunt infection. Leukocytosis and increased CRP levels supported the presence of inflammation and culture grew Staphylococcus aureus. The patient improved with Clindamycin therapy. To our knowledge, this is the first AST case preceded by hemodialysis AV shunt infection.
Key words: acute suppurative thyroiditis, hyperthyroid, chronic kidney disease, arteriovenous shunt, haemodialysis
Thyroiditis is inflammation of the thyroid that can be caused by an autoimmune disorder, as well as viral, bacterial, fungal, and other infections.1 Acute suppurative thyroiditis (AST) is rare, accounting for only 0.1%–0.7% of all thyroid disorders. AST is more common in patients with Hashimoto’s thyroiditis and thyroid cancer. A predisposition is associated with the persistence of ducts originating from the 3rd or 4th bronchial sac which can lead to recurrent abscess. Most infections spread to the thyroid gland via a piriform sinus shunt. The left lobe of the thyroid gland is more commonly affected. AST can be life-threatening with a mortality rate of 12% or more due to thyroid storm and sepsis.2 The diagnosis can be delayed due to atypical clinical features. AST is rare because of the bactericidal nature of colloidal materials, increased vascularity, and the presence of iodine. A thyroid abscess presents as a very painful swelling. The differential diagnosis for thyroid gland pain is subacute and chronic thyroiditis.3
A 40-year-old woman was admitted to the hospital with the chief complaint of swollen neck pain for 2 days, accompanied by difficulty swallowing and fever. The patient had never had the same complaint before. One week previous, the patient had surgery due to infection in the AV hemodialysis shunt. The patient had a history of chronic kidney failure (CKD) stage V for one month and underwent hemodialysis twice weekly. The patient had hypertension for about 7 years, but there was no history of diabetes mellitus or thyroid disorders.
Clinical Findings (upon arrival to ER)
The patient was generally weak, but conscious (GCS 4-5-6), with blood pressure 110/70 mmHg, pulse of 92/minute, respiration rate of 20/minute, and axilla temperature of 38°C. Other physical findings revealed left anterior swelling of neck which was warm and tender, size 4–5 cm, moving up and down when swallowing, and painful (Figure 1).

Figure 1. Swollen and painful left side of the neck of patient.
Diagnostic Assessment
The patient underwent laboratory testing including serial hematologic testing, clinical chemistry testing, and thyroid hormone function testing (Tables 1–4).
| Parameter | Day 5 | Day 7 | Ref Range |
| HBsAg | Non Reactive | - | - |
| HIV | Non Reactive | - | - |
| ANA tets | - | 24.56 | - |
| C3 (mg/L) | - | 85 | - |
| C4 (mg/dL) | - | 49 | - |
Ultrasonography (USG) of neck showed an abscess involving the entire left lobe of the thyroid with a size of 3.54 x 2.2 x 5.49 cm. A smear from a Fine Needle Aspiration Biopsy (FNAB) contained a distribution of lymphocytes and polymorphonuclear (PMN) cells as well as macrophage cysts against a broad erythrocyte background. The pathological diagnosis was acute suppurative thyroiditis (Figure 2). Culture of the pus grew Staphylococcus aureus sensitive to gentamycin, ampicillin-sulbactam, oxacillin, cotrimoxazole, erythromycin, clindamycin, quinupristin-dalfopristin, levofloxacin, moxifloxacin, but resistant to ampicillin and tetracycline.
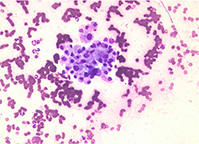
Figure 2. FNAB Results Show an AST
The patient was treated initially with ceftriaxone, 1g every 12 hours, then on day 12 changed to clindamycin oral, 300 every 12, when the culture and sensitivity results became available. The head and neck surgeon planned to perform incision-drainage of the abscess after patient had become stable and had normal thyroid function. This patient also received amlodipine oral 10mg per day, paracetamol 500mg oral, thyrozol 10mg oral, propranolol 10mg oral, folic acid 1mg oral, and haemodialysis as scheduled 2 times/week.
On follow up, the patient was clinically well with no fever. The patient’s abscess was drained at day 31.
Abscess formation frequently occurs in children due to anatomic abnormalities such as piriform sinus fistulas. Thyroid abscesses in adults are extremely rare and may be caused by foreign body trauma (FNAB, fishbone) and anatomical pressure. Hematogenous spread from distant sites is known to be the most common cause of thyroid infection, although the exact mechanism is unknown. The manifestation of thyroiditis is mostly local pain in the involved lobe, accompanied by pain and difficulty of swallowing. Symptoms of fever and chills may occur depending on the virulence of the microorganism and the occurrence of sepsis. 1-2,4-8
Primary thyroid abscess from AST is a rare type of head and neck infection because the thyroid gland is known to have infection-resistant mechanisms. Thyroid protection includes a rich blood supply and lymphatic drainage, high iodine content of the gland which is bactericidal, separation of the gland from other neck structures by the fascial plane, and formation of hydrogen peroxide within the gland for thyroid hormone synthesis. AST is usually more painful than in patients with subacute thyroiditis. Subacute thyroiditis usually displays as severe localized tenderness, but is less likely to be thyrotoxic (60% of patients).1
This patient had left neck lump pain followed by fever, and difficulty in swallowing. It was suspected that there had been hematogenous spread of bacteria creating thyroid infection because the patient had just had an AV haemodialysis shunt transfer operation 1 week earlier. Prior to the surgery, the patient experienced fever, chills, and the left AV haemodialysis shunt was starting to have a red and painful swelling. The patient had had a pseudoaneurysm repair related to prior AV shunt infection.
The patient had leukocytosis and elevated CRP that supported signs of inflammation. High FT4 levels and low TSH levels indicated a hyperthyroid condition. Hyperthyroidism in thyroiditis may occur naturally over weeks to months. These patients should be treated immediately because AST is a life-threatening condition (12% of mortality if not treated immediately). Mortality may occur in result of thyroid storm and sepsis. Thyroid storm develops when hyperthyroidism is not treated, resulting in symptoms of fever, increased pulse, blood pressure, nausea, vomiting, and agitation.
Ultrasound examination revealed an abscess in the thyroid gland or evidence of lobe enlargement, while FNAB determined the presence of infection, done simultaneously with culture.1 The patient’s ultrasound showed an abscess involving almost the entire left lobe of the thyroid with a size of 3.54 x 2, 2 x 5.49 cm. FNAB results showed that the smear contained the distribution of lymphocytes and PMN cells and cyst macrophages with an erythrocyte background; no signs of malignancy were found.
Drainage-incision of the thyroid abscess was planned after euthyroid status had been achieved. Basic incision and drainage is a necessary surgical procedure as therapy, but care must be taken to treat hyperthyroidism first to avoid postoperative thyroid storm and other unwanted metabolic effects. Although this condition is rare (0–14%), the clinician avoided the possibility of a thyroid storm.9 Therefore, in the early stages, the clinician recommends giving antibiotic and antithyroid therapy to treat thyrotoxicosis.
Appropriate antibiotics should be given accordingly to the causative organism. Culture of the aspirate of this patient exhibited significant growth of Staphylococcus aureus. The patient came to the hospital and received an injection of ceftriaxone 1gram intravenous daily for two days as empiric treatment. Furthermore, after the results of the culture antibiogram were released, the patient’s antibiotic was changed to clindamycin, 300 mg orally twice a day, starting on the 14th day. Several previous case reports showed that the bacteria causing thyroid abscess was methicillin-resistant S. aureus (MRSA) which was not sensitive to ceftriaxone.10 The culture results in this patient showed sensitivity to oxacillin, indicating that this S. aureus was not MRSA. The oral therapy given was Clindamycin, because this drug is safe for CKD patients.
The patient also suffered from CKD which is able to cause immune system disorders. Disorders can be in the form of systemic inflammation and immunosuppression.11 There is an increase in proinflammatory cytokines in CKD such as pentraxin, in addition to dysfunction of phagocytes, B and T cells.12-15 Haemodialysis therapy is the key to improving the general condition and the patient’s immune system.
The patient had incision and drainage done after thyroid function became normal. The prognosis is excellent with maintenance of normal thyroid function; however, post-thyroiditis thyroid function tests should be monitored to ensure that a thyroid disorder is not ongoing.
To our knowledge, this is the first case report of suspected haemodialysis AV shunt infection causing hematogenous spread to the thyroid organ leading to AST.
The patient was diagnosed with AST that was probably caused by post-infectious AV shunt-haemodialysis. We recommend that cases of neck swelling and fever after infection with AV haemodialysis shunt undergo a thorough thyroid testing, ultrasound, and FNAB for early diagnosis of AST, and timely treatment because of its life-threatening nature.