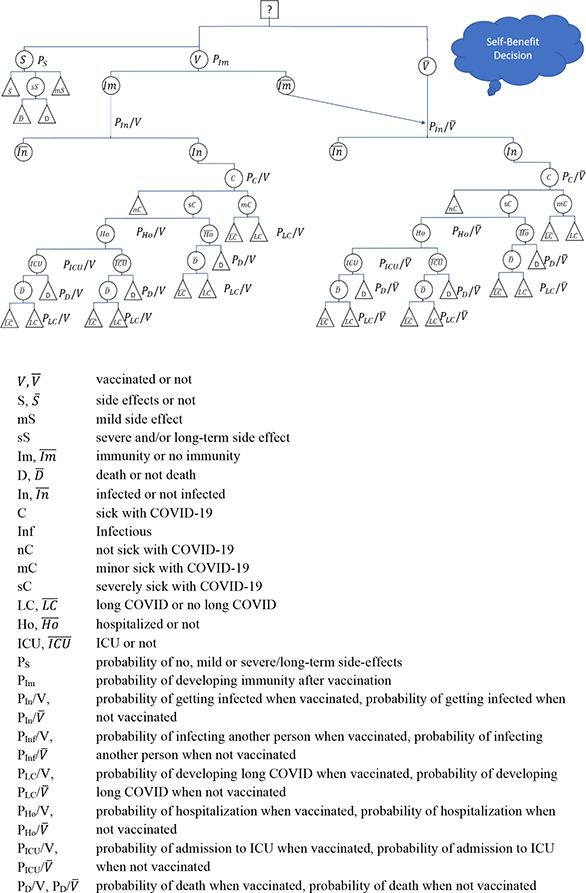
Figure 1. Self-benefit Decision on Vaccination against COVID-19. Source: own.
COMMENTARY
Steffen Flessaa
a PhD, Professor, Department of Health Care Management, University of Greifswald, Germany
The Covid-19 pandemic inspired a fierce discussion on pros and cons of vaccinations among Christians. Frequently, this emotional dispute is not based on facts, and this might be due to the fact that the decision situation (“to be vaccinate or not to be vaccinated”) is quite complex. In this paper we develop a risk-analytic model of the vaccination decision and explain the benefits of vaccinations against SARS-Cov-2 on different levels. Furthermore, we show that the Great Commandment of love calls for avoiding all harm to the neighbor even if this harm is indirect and under uncertainty. Consequently, it is a Christian duty to love one’s neighbor and be vaccinated.
Key Words: COVID-19, Christian duty, love, risk-analytical model, decision-making
A vaccination against an infectious disease is one of the most effective, efficient, and safe instruments to protect the health of a population. Based on vaccines, smallpox1 was eradicated and other pandemic diseases such as measles2 and polio3 were substantially reduced. Before the dawn of the vaccine era, millions of lives were lost annually, and many more were severely affected by suffering and long-term disability; these diseases have lost their horror today.4 It is estimated that measles alone killed 2-3 million children every year before global vaccination programs were introduced in the 1960s. Only some 140,000 died in 2018 due to the disease—almost exclusively unvaccinated children under five.5 The only reason why measles has not been eradicated yet—as envisioned by the World Health Organization (WHO)—are niches of unvaccinated people.
Vaccinations are seen as the most effective, efficient, and safe form of prevention,6 and they are much more cost-effective than any treatment. As most of the “big killers” are contagious, other forms of prevention would require social distancing, which is very difficult to implement in the long run, in particular for children. Treatment of patients is frequently not precise as we have only a limited portfolio of therapeutics against these viral diseases. Consequently, early vaccination is the most rational approach, strongly encouraged by the United Nations, WHO, all Ministries of Health, and Christian organizations7-9 involved in health care. There is a steady increase of recommended vaccination targets, including rotavirus disease, human papillomavirus infection, and hopefully, malaria in the near future. After having given billions of vaccinations to billions of people in decades, we can state that there is hardly any medical intervention which has been so thoroughly analyzed, for which we have such a broad empirical basis, and which has proved to be as safe as vaccinations. In addition, vaccine technology has undergone progressive improvement such as tissue culture vaccines for rabies, high potency killed vaccine for polio, and mRNA technology that promises future improvements in many areas.10 Negative side effects exist, but they are a small fraction compared to the risks of contracting the respective disease.
One of the most distinguishing features of vaccinations is that they can eradicate a disease completely, as long as the disease does not have other natural hosts or reservoirs. For instance, eradicating yellow fever will require eradicating the virus not only in the human population but also in the monkey population. As long as this population still serves as a reservoir, a reinvasion into the human population will always be possible. However, many other diseases, such as polio or measles, could be eradicated, such as smallpox, if we just managed to get all human beings vaccinated for several years. After the last case will have been healed or died, the disease would be gone forever and future vaccinations against it would be needless. There is nothing as sustainable as eradicating a disease—it would require “simply” the will, financial resources, and management to implement a global vaccination program without niches where the agent can persist.
However, until today, these niches refuse to be vaccinated. A rather small number of people is sufficient to build up a reservoir for the disease so that it can persist and constitute a constant threat for the entire world. Some of these populations have convictions that prohibit vaccinations, others are undecided and hesitate to gather sufficient information for making an informed decision. For instance, anthroposophical communities assume that a child needs viral or bacterial insults to develop properly. Thus, they refuse to be vaccinated.11 Other niches are communities and areas of Christians who reject vaccinations for religious reasons. For instance, a few hundred thousand orthodox protestants in the so-called “Dutch Bible Belt” in the Netherlands reject vaccinations and report the highest numbers of measles cases in the entire country.12 Even a simple mapping reveals that the geographical distribution of this Christian group and the measles cases in the Netherlands clearly shows that this group is the main driver of periodic measles outbreaks. Just as described elsewhere for the situation before the introduction of the vaccine (e.g., prominently about measles in Iceland), the disease comes in waves, infects almost the entire population of children without vaccination and immunity during an outbreak, and then disappears just to come back after a few years when a sufficient number of children have been born who are not immune.13 As soon as one measles case comes into the population from outside, the epidemic is likely to start again, i.e., the measles pandemic is sustained jumping from niche to niche, for instance, from the orthodox protestant Christian community to Christian communities all over the world. The results are not only fatal cases and severe morbidity, but also a high risk for the small population outside this community who cannot be vaccinated for health reasons. It seems that vaccine refusal is highly associated with “religious or philosophical reasons.”14
In this paper, we will argue from a social ethics perspective15, i.e., it is not our intention to provide physicians with instruments to give counselling for individual patients hesitating to be vaccinated. Instead, we would like to contribute to the general discussion on a macro level and reflect on the question whether being vaccinated against a life-threatening disease is a Christian duty. For this purpose, we develop a risk-analytic model demonstrating the decision situation of an individual considering only his utility or the good of others and the society based on the example of coronavirus disease 2019 (COVID-19). Afterwards, we will discuss the potential benefits of vaccination against COVID-19. We realize that the decision to be vaccinated also depends on our understanding of the Great Commandment to love one’s neighbor as oneself. Consequently, we analyse the scope of this commandment. The paper closes with some conclusions.
In this section, we would like to analyze the decision situation of an individual who has to decide to be vaccinated against COVID-19 or to reject the vaccination. For this purpose, we use a decision tree as it is frequently used in medical decision making, in particular on a macro level.16,17 The purpose of this model is to increase the transparency about decisions (“arms”), probabilities, and results on a macro level. As stated before, the model is not intended to be used as a decision-making tool for individual counselling of a patient, but as an instrument to assess the nature of the decision-situation in the sense of “modelling for insights, not for numbers.”18
Figure 1 exhibits the decision situation for an individual focusing only on his own utility (“self-benefit decision”). V stands for the decision to be vaccinated, V for not being vaccinated. If the person is vaccinated, he can suffer from severe side effects (sS), mild side effects (mS) or no side effects (S ) with the respective probabilities (PS). In the case of severe side effects, even death (D) is possible. At the same time, the person develops immunity (Im) with a probability of PIm Im determining the likelihoods of all further events. In both cases, the person can be infected by SARS-CoV-2, but for the immune, the probability to get infected when vaccinated (Pin/V) is much lower than for the non-immune (either because he was not vaccinated at all or because he did not develop an immune response). The probability of being infected does also depend on protection measures, such as wearing of masks (which can considerably reduce the risk)19 and the contact frequency, but these interventions exist irrespective whether somebody is vaccinated or not.
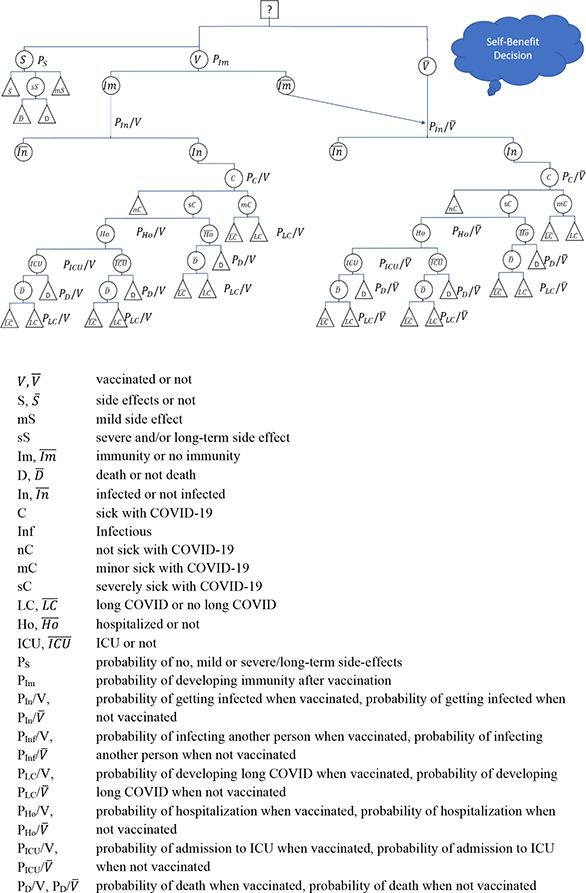
Figure 1. Self-benefit Decision on Vaccination against COVID-19. Source: own.
If the vaccinated is infected, he will get COVID-19 symptoms (C) with a probability of PC/V as a mild case (mC) or a severe case (sC), but also the mild case can develop long COVID (LC) with a certain probability PLC/V. A severe case can be admitted to a hospital (Ho) or intensive care unit (ICU), and severe and mild symptomatic cases can die or develop long COVID. The respective probabilities depend on the branch of the decision tree.
The probability tree of a non-vaccinated person is identical with the tree of vaccinated without immune response (right-hand side) and mirrors the situation of an immunized but with different probabilities. For instance, the risk of a person vaccinated with Comirnaty© (BNT162b2, vaccine against SARS-CoV-2 of Pfizer-BioNTech) to get infected is about 50 % of the respective statistic of a non-vaccinated,20 the risk of developing symptomatic COVID-19 is only about 30 %, the likelihood of being hospitalized is less than 20 %, of being admitted to an ICU is less than 10% and of dying less than 2 % of the respective statistic of a non-vaccinated.21,22 The precise figures depend on the age and health condition of the vaccinated, the time after the vaccination and the virus variant, but in all cases, the arm of the vaccinated has much lower probabilities of developing severe disease symptoms than the arm of the non-vaccinated. However, the arm of the vaccinated also includes the branch of developing side effects of the vaccination from very mild to death.
Figure 1 shows the decision situation for an individual who does not consider the impact of his decision on others. We call this a self-benefit decision. However, it is a decision with uncertainty as all arms contain probabilities. There is no decision without risk, but from all that we know from the literature, the expected value of individual suffering (morbidity and mortality) is lower if a person is vaccinated. At the same time, the range of possible events, as well as the standard deviation of the results, are not higher for the vaccination arm. Consequently, it is rational to go for vaccination even if one considers only his own life. However, the model clearly shows that the decision situation is highly complex. Many arms have to be compared, many probabilities have to be sought from the literature, and many results of possible events have to be discussed. Consequently, an individual might be overburdened with the decision situation.
Decision-making involving uncertainty and incomplete information can be difficult for the individual. However, very often the individual trusts experts when he is overwhelmed with a risk analysis. For instance, most people are not experts in metabolism, but they trust the medical experts that high levels of cholesterol are dangerous; consequently, they behave accordingly. Trusting experts is a normal strategy to overcome uncertainty and incomplete information.23 A frequent alternative is “doing nothing”—in this case, avoiding the immunization because the risk of infection is in the future while the risk of getting side effects exists today. Furthermore, an irrational decision-making process of ignoring risks might be acceptable for an individual, but it is definitely not for the policy-makers, also not for leaders of churches and Christian health care organizations. They can be expected to make informed decisions for the best of the people entrusted to them.
Figure 2 shows the decision situation for a person considering explicitly the impact of his vaccination decision on the lives of others. He knows that once he is infected himself, he can infect others. The likelihood of infecting another person is expressed as Pinf/V if the person is vaccinated and Pinf/V if he is not vaccinated. There was the hope that Pinf/V would be zero, but it is a matter of fact this is not valid for the Delta-variant. For instance, Singanyagam et al. found that there were no differences in the peak viral loads between unvaccinated and vaccinated individuals.24 Likewise, Brown et al. speculated that the viral load of vaccinated and unvaccinated persons infected with SARS-CoV-2 are rather similar.25 However, Elliott et al. estimated an effectiveness of the vaccine against COVID-19 infection of 49% (with an effectiveness against symptomatic infection of 59%).20 Mallapaty also concludes that “growing evidence finds that they [vaccines against COVID-19] also substantially reduce the risk of passing on the virus SARS-CoV-2.”26 The reason is—most likely—that while the peak viral load between vaccinated and non-vaccinated might be similar, the overall viral load of vaccinated is lower as vaccinated people clear the virus more quickly, i.e., “within days of infection, the viral load in vaccinated people drops much more rapidly and therefore makes them much less likely to transmit [COVID-19].”27 Consequently, Maier et al. found that “67%–76% of all new infections are caused by unvaccinated individuals” in Germany (autumn 2021,)28 although merely some 30 % of the population were unvaccinated. Thus, we can conclude that vaccination reduces the risk of infecting others, i.e., 0 < Pinf/V < Pinf/V.
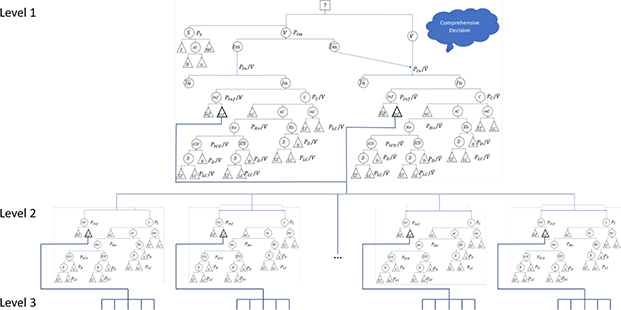
Figure 2. Comprehensive Decision on Vaccination against COVID-19. Source: own.
Once another person is infected, the entire decision model starts again. As we do not know whether the other person is vaccinated or not, the model does not differentiate the two arms at the next level. This could be done, but it would make the model even more complex. The other person might himself infect another person (level 2) who himself might infect others (level 3 etc.). While the wild variant of SARS-CoV-2 had a much lower basic reproductive rate29,30, the delta variant has an R0 of about five, i.e., each infected person31 will—on average—infect another five. In other words: A comprehensive decision model will require considering at least the arms, probabilities, and results of five different persons. If we consider several levels of infections and take responsibility for everybody who can trace his infection back to the decision-maker, the number of infected whom we have to consider in our decision grows exponentially.
Summarizing the insights of the risk-theoretic decision model, we can state that the decision to be vaccinated or not to be vaccinated will depend on several variables:
COVID-19 has negative consequences for the individual, for communities, and for societies. Consequently, reducing the likelihood of being infected (by a vaccination) has a number of benefits. However, the relevance of these harms and benefits for the decision-maker depends on the decision concept. If a decision-maker focuses only on his self-benefit interest, only a few decision criteria are relevant. If he focuses comprehensively on other people, the number of criteria is manifold. Table 1 shows the relevant decision variables.
For the patient himself with a self-benefit concept, the prime focus is the assessment of pain, fear, sorrow, and death during the period of acute sickness and possibly during the long-term recovery as represented in Figure 1. These are essential elements of intangible harm, but the patient might also face co-payments and out-of-pocket payments depending on his insurance coverage. At the same time, some indirect costs might occur. For instance, the person will be unable to work for some time and might lose income (depending on the social protection system). Students might miss some classes and might have to repeat a year of training. However, the main criterion for a self-benefit decision-maker is his own health.
A more comprehensive decision-maker will include those people he might infect, as shown in Figure 2. Thus, not only the pain, fear, sorrow, and death of the decision-maker, himself, but also of all possibly infected will have to be included. As those whom he infects will infect others again (shown as level 3 in Figure 2), the decision-maker has to consider how many levels he will include in his decision, i.e., he has to decide whether he considers only those whom he infects directly or all who can trace their infection back to him. As stated above, the basic reproductive rate (R0) expresses the number of individuals one person (on average) will infect if no immunity exists. If i denotes the number of levels one person will consider, the number of infected he will have to consider is Ri0. For instance, at a level of i=2 and R0=5 (delta variant), the decision-maker will have to consider the pain, suffering, death, financial hardship, and indirect cost of 25 people, for i=3 already 125 people. For the wild variant with an R0 of about 2.5,29 the respective figures are 6.25 and 15.63, i.e., the issue of “comprehensive decision-making” and considering further levels in the infection chain has strongly been enforced by the new variant(s).
A special group, which could be included in the comprehensive decision-making, are the health care services and their staff. COVID-19 has brought health care staff, in particular doctors and nurses of ICUs, to their limits. Many are overwhelmed, have experienced tremendous stress, and feel guilty in a situation where they cannot help anymore. The number of nurses who have given up their job during the COVID-19 pandemic is high. Others have been infected during their duty, and in particular at the beginning of the pandemic, doctors and nurses were among the highest risk groups.33,34
COVID-19 does not only have an impact on the staff but also on other patients. The capacities used to treat COVID-19 patients are missing to treat others, and frequently, elective surgeries had to be postponed, and other patients were not treated well as usual. Any additional COVID-19 case also means additional risk, hardship, and potential harm for health care staff and patients with other diseases.35
The widest concept of decision-making will consider the impact of the disease on the entire society. During the months of the pandemic, many societies have seen a negative impact on the entire society. Some have developed a high degree of mistrust against the Government. In Germany, for instance, a movement called “Querdenker” has developed. They insist that SARS-CoV-2 does not exist and that COVID-19 is a lie of the government to control the people. Thus, they fight against governmental programs to control the disease. The German intelligence service assesses the movement as extremely right-wing with the potential of conducting violence against officials. Others have lost interest in politics, as they are frustrated with all the interventions against the disease.36
Another societal consequence of the disease are the high costs of treating patients. Some health insurances, but also hospitals, have come close to bankruptcy because the normal rebates and premiums cannot refinance the high costs of COVID-19 patients. Other institutions have to train new staff because the existing personnel have left their jobs. The highest societal costs are usually caused by complete lockdowns including strong subsidies for enterprises affected (e.g., tourism, entertainment). For Germany alone, it is estimated that each week of lockdown cost some 3.6 billion Euro37 — and the lockdown lasted for months.
The long-term consequences of COVID-19 are still unclear. For instance, the early and uncoordinated closing of borders between EU countries in the Schengen area (e.g., between Germany and France) in March 2020 caused tensions between the countries and might cause long-term damage to the international relations.
The societal costs are partly caused by each additional infection. Every individual has to consider his contribution to the achievement of herd immunity, which is achieved if the net reproductive rate (N0) is less than one. N0 considers the share of the immune in the total population, i.e.,
N0 = R0(1 – n)
where n denotes the share of the immune population. The epidemic comes to an end if N0<1 or
In this case, n denotes herd immunity, i.e., the immunity level in a population that is required to stop the epidemic. For instance, a COVID-19 epidemic with R0=5 will come to an end if n>0.8, i.e., at least 80 % of the population becomes immune by vaccination before the epidemic stops. Assuming that existing vaccinations protect only by 90 %, the realistic vaccination rate must be at least 89%; if it protects by 80%, the entire population must be vaccinated.*
Consequently, if a vaccine protects by less than 80% against the infection (and being infectious) with the Delta-variant, herd immunity will not be reached,38 and there is some doubt whether herd immunity could be reached at all for COVID-19.39 Does this mean that a comprehensive decision-maker should not consider the next levels of infection and his contribution towards herd immunity (even if it is never reached)? As long as Pinf/V < Pinf/V, we can state that a vaccination against SARS-CoV-2 reduces the risk of infecting others and lightens the burden of the disease for individuals and the society. Protecting the contact persons of the next level, the health care services, and the society might not be perfect, and the disease might not be eradicated completely (in particular as it is not perfectly clear whether a re-invasion from the natural reservoir of bats is feasible), but everybody can contribute to struggle in the right direction.
Thus, a decision-maker who considers the societal harm of COVID-19 will have a strong drive to be vaccinated and to contribute to herd immunity to avoid the societal harm of the disease.
As stated above, every decision-maker has to decide on the level considered, the assessment of the results, the probabilities, and the way of dealing with the complexity. Most crucial is the question of whether a decision should reflect only the benefits and harms for the decision-maker himself or other people as well. For a Christian, it should be clear that the life of other people (“the neighbor”) is relevant as well, i.e., a purely self-benefit decision is unacceptable for a Christian. However, in reality, the situation is not as easy as the different arms of the decision tree are all subject to certain probabilities, and this decision situation seems to be unusual for many Christians.
Like in most other ethical reflections, there is no direct commandment in the Bible that gives an unequivocal instruction to be vaccinated or not. Instead, Christians have to reflect a decision-situation in the light of the facts (in particular, provided by science) and Biblical values. While specific commandments might be time-bound and limited in scope, the values underlying the Biblical illustrations (such as peace, freedom, justice, love, forgiveness) are relevant for Christians as their decision variables in a concrete situation although they will require ethical consideration.40 It is our responsibility to reflect on their relevance in a concrete situation.
We assume that there is general agreement that the “Great Commandment“ (Math. 22: 37-38) is the core of Christian duty, i.e., to “love the Lord your God with all your heart and with all your soul and with all your mind [… and to] love your neighbor as yourself.” The last part (“Ἀγαπήσεις τὸν πλησίον σου ὡς σεαυτόν”) refers to the Ancient Greek agape-love (ἀγάπη) as the selfless and unconditional love, distinct from brotherly love (philia, φιλία) and sensual love (eros, ἔρως). Agape is seen as the highest Christian virtue.
Paul also writes that we have no duty except to love (ἀγαπᾶν!) each other as all commandments are fulfilled in this one (Rom 13: 8). Consequently, love is the only Christian duty, and love is the criteria to analyze whether a Christian should support vaccinations or reject them. If love calls for vaccination, it is the duty of the Christian to be vaccinated and to help others to be vaccinated.41,42
However, the term love is not easy to define, and it is not operational enough to use it as decision criterion without further reflection. Consequently, we have to ask what love actually means in a biblical context and what it could mean concerning a vaccination program. For this purpose, we start with an understanding of love where we can meet general agreement: Murdering another person is against love. Consequently, the fifth commandment (Exodus 20: 13) expresses it clearly and unequivocally. The sense of this commandment for individual well-being, but also for social cohesion, is self-evident. Nobody should raise his hand, ax, pistol, or rocket to cause damage to another's body that would lead to death. In the small catechism, Luther extends the range of the commandment when he demands, “that we do not hurt or harm our neighbor in his body, but help and support him in every physical need.” Thus, this commandment covers not only the direct and intentional murder but also careless harm or putting at risk. Furthermore, it does not only prohibit human actions that are immediately and likely to lead to harm, but also anything that does not “help and support him in every physical need.”
Physical injury and death can also occur unintentionally, indirectly, and with a certain probability under uncertainty. The driver who drives through zone 30 in front of a primary school at 80 km/h has no intention of running over a child, nor is he sure to kill someone while driving. However, he takes (consciously or unconsciously) the risk that someone will be harmed by his action. We see this person ethically and legally responsible for damage if he caused it negligently. Moreover, most people share the opinion that Christian love calls for responsible action to reduce the risk to harm children.
While most would agree that risking the life of a child by driving tremendously irresponsible and breaches the commandment of love, it is not as clear that any hazard constitutes a violation of the principle of love. If someone wants to avoid completely any risk of jeopardizing the life of other people, he must not participate in road traffic, restrain from most social activities, and definitely not become a doctor or nurse who are always at risk of harming other people. In particular, those activities we usually associate with love (e.g., heal, feed, visit others) increase the risk of harming and, consequently, breaching the commandment of love. It seems that we accept a risk if the damage occurs only with a certain probability and if the alternative is worse. In other words: Christians have to analyze which alternative has the lowest expected value of breaching the commandment to love the neighbor. Then Christians have to choose this alternative in the knowledge that there is still a risk of harming others.
Jesus underlines the importance of love by making it a distinguishing feature of Christians: “A new command I give you: Love one another. As I have loved you, so you must love one another. By this, everyone will know that you are my disciples if you love one another” (John 13: 34-35). To be a Christian means to love, a Christian existence without love would be a contradiction in terms. The Bible bases this love on the fact that God loves his creatures to the point of self-abandonment (Rom. 8: 31-36; John 3: 16). The task of the Christian is to pass on this love because faith without deeds of love is dead (Gal 5: 13; James 2: 17; 1 John 3: 17).
From a biblical perspective, however, love is primarily not an emotion, but an action, as is shown, for example, in the parable of the Good Samaritan (Luke 10: 25-37). The narrative does not describe any emotion, but gives—despite all the complexity and challenge of the narrative43—an instruction to act in the same way. The eschatological speech of Jesus (Mt 25: 31-41) also emphasizes love for the weak and helpless, which is expressed in concrete actions, e.g., looking after the hungry and thirsty, taking in strangers, clothing the naked, and visiting the sick and prisoners. Love appears in this—certainly not exhaustive—list as a rational act, not as an emotion. This active love even becomes the criterion for entering the kingdom at the right hand of God (Mt 25: 31-36) and definitely includes rational decision-making with a comprehensive analysis of different arms, probabilities, and levels of the decision.
A strong focus of the “works of mercy” is health in its wider sense. It includes the physical (hunger, thirst, nakedness), the social (visits, reception), and the mental dimension of health which are also referred to in the definition of health in the constitution of the World Health Organization.44 However, health in the biblical sense goes beyond these three dimensions and also includes a spiritual dimension, since “shalom” is only possible in communion with the creator.45 Thus, health in the Christian understanding is the goal of love, but in a comprehensive sense that includes the active creation of relationships, meaning in life, joy of life, peace, and justice as well as spirituality. Love is never self-benefit, but notoriously comprehensive and people-oriented. It looks for the best for the neighbor and the entire society as a prerequisite of a healthy life for the neighbor.
Consequently, Christian love is action-based, comprehensive, and reflective. It would be insufficient to base love on emotions and reduce it to avoid direct harm to people in front of me. In the parable of the Good Samaritan, the scribe originally asked: “Who is my neighbor?” (Luke 10: 29). So he asked from himself, from his point of view, from his intention. Jesus tells the parable and then turns the question around: “Which of these three do you think became a neighbor to the man who fell into the hands of the robbers?” (Luke 10: 36). Jesus is concerned with the experience of neighborly love from the point of view of the helpless, i.e., a rather rational and result-oriented point of view.
We can, therefore, state that the endangerment of people can represent a breach of love, even if its materialization is subject to a certain probability. Drivers running at 80 kilometers an hour in zone 30 in front of an elementary school are not only breaking the law, but they also violate the principle of love because they neglect the possible consequences of their actions for those whom they are called to love. An HIV-positive man who, against better judgment, has unprotected sexual intercourse with another person unaware of this risk does not only commit (attempted or completed) physical harm, but also acts in an absolutely loveless manner because he knowingly endangers the life of another person. Consequently, a Christian must consider the consequences of his decisions for all potential neighbors even if the risks are subject to probabilities.
Based on our reflections on Christian love and the risk theoretic decision model of vaccination against COVID-19, we can state that Christians must also consider the long-term, indirect, and uncertain consequences of their decision to be vaccinated or to reject the vaccination. This reflection will also include the risks of harming other people. It is the Christian duty to love one’s neighbor, but not only those standing directly in front of me and those I may damage face-to-face, but also the anonymous ones I might kill or harm with my decision.
COVID-19 is a disease with tremendous potential to cause suffering, sorrow, and costs on an individual and societal level. This harm can be grossly avoided by a vaccination, and the spread of the disease can be stopped if only a sufficient number of people are vaccinated. A Christian must take a societal perspective in his decisions because he is called to love his neighbor.
Rejecting the vaccination against COVID-19 is also quite haughty because it considers neither the complexity of the decision situation nor the recommendations of the experts. Christians should love their neighbors in humility—and humility calls to accept the opinion of the experts in particular when they are Christians themselves. If a person who is not expert in virology and epidemiology himself does not pay attention to what the experts say and simply rejects their expertise, he is guilty of arrogance that leads to a breach of love. In former times, arrogance was considered a “mortal sin”—a term that might sound obsolete. Nevertheless, rejecting the expertise and good reasoning of experts breaches the commandment of love if it leads to harm, suffering, and death of our neighbor.
Here, we have to repeat that this paper argues from the perspective of social ethics asking the question what is generally “right” or “wrong” from a macro perspective. Counselling of an individual (patient) will require totally different approaches and instruments as there is frequently a gap between societal ethics and approaches of individual behavior changes. On an individual level, addressing arrogance might lead to blaming, while neglecting arrogance on a social, non-individual level might be misleading a decision-making process of high relevance for the society as a whole. Therefore, it is important to distinguish individual counselling and social ethics.
From a perspective of social ethics, to love one’s neighbor requires reflecting on the consequences of our decisions on them even if these consequences are subject to certain probabilities. We do this when we participate in traffic or when we engage in our professions. Life is not without risks, but Christians should always consider the impact of their life on others. Based on love for the neighbor, Christians have to apply a comprehensive concept of decision-making (see Figure 2), consider the impact of their vaccination decision not only on themselves but also on the community and society (see Table 1), and invest effort to reduce the risk of harm for all images of God. Based on this concept of love, a vaccination against COVID-19 is a Christian duty.
In this paper, we do only address the macro level of social ethics. More research has to be invested in the most appropriate way to convince individual Christians hesitating to be vaccinated. Furthermore, anti-vaccine attitudes of certain Christian groups that compromise herd immunity have to be addressed in a joint effort of theology as well as political and sociological sciences.46 Consequently, this paper finally calls for more collaborative research on vaccinations from a Christian perspective. Whether an increased theological, medical, and scientific knowledge will indeed convince these groups or whether they will be trapped in an irrational rejection of vaccinations is also beyond the scope of this paper. However, this analysis clearly demonstrates that a rational Christian decision-maker will perceive vaccination against COVID-19 as a Christian duty.
* If an infection with SARS-CoV-2 produced life-long immunity, the number of COVID-19 cases would have to be added. However, this is not fully the case. Instead, it is recommended that former cases of COVID-19 should be vaccinated as well after six months in order to have a full and lasting immune response.