FIELD REPORT/BRIEF COMMUNICATION
Samone Franzesea, Carolyn O’Brienb, Doug Fountainc
a MD, MPH(c), Johns Hopkins Bloomberg School of Public Health, USA
b MSPH (International Health), Program Advisor, Christian Connections for International Health, USA
c MPA, Executive Director, Cristian Connections for International Health, USA
Faith-based organizations (FBOs) provide a significant portion of healthcare services in low- and middle-income countries (LMICs), but the scope and scale of these services are difficult to track, leading to decreased understanding and integration of services with host-country assets. This analysis looks at the current understanding of FBOs’ reach, their limitations, and the role that the newly formed Christian Health Asset Mapping Consortium (CHAMC) hopes to fulfill. CHAMC is a voluntary association of organizations that will work to address urgent needs for information on and help improve the quality of data about the Christian health asset landscape.
FBOs provide healthcare services via faith-owned health facilities, congregations, community-based organizations, and national and international organizations.1-2 Their scope includes clinical services at primary, secondary, and tertiary levels, as well as preventative care like immunization initiatives and cancer screenings, disaster preparedness, HIV/AIDS education and medical care, maternal and newborn care, emergency care, family planning services, and more.3-9 FBOs also run training institutions for different cadres of health and allied-health care workers.
FBOs are poised to continue to provide a substantial amount of the healthcare services in LMICs and have a profound impact because of their remote locations, long term commitments, influential role in communities, and ability to reach and connect with hard-to-reach populations. FBOs operate in austere and underserved populations and are sometimes the only entry point for rural populations.3,5 Furthermore, FBOs are frequently rooted in the communities in which they work and are, thus, able to implement interventions that take into account the local culture and customs.11 In addition to FBOs, clergy, and other religious leaders have strong voices in communities and help promote health and wholeness in areas such as vaccine access and acceptance and family planning services.9,11-12 In one study, contraceptive use was 1.7 times higher in women whose religious leaders discussed family planning compared to women who were not exposed to family planning discussions in religious settings.13
While there is potential for FBOs to have this profound impact, there are multiple limitations in FBOs’ health service delivery that need to be addressed, including identifying sustainable funding structures, integrating with national health services, and complete documentation of FBO services throughout LMICs. For effective health system strengthening, FBOs should try to partner with government organizations to fill gaps as needed and focus on building capacity.14-15 While some governments have working relationships with FBOs, other governments struggle to integrate FBOs into the healthcare system. While there are many ways governments can have relationships with FBOs, an example of a robust partnership is in Ghana, where the government funds over 70% of the work of the Christian Health Association of Ghana facilities. In contrast, we understand that partnerships between FBOs and local governments are not always possible due to the political climate. Still, partnerships among faith actors are possible in these instances.
There are also significant limitations of our knowledge of FBOs, to include the number and location of community-based health programs and preventive services, the scope and capacity of faith-affiliated health worker training institutions, and the status of supply chains that serve faith owned (and all private non-profit) health services.
The lack of understanding and quantification of the scope and practice of FBOs is a pressing need for FBOs. Olivier et al.1 is often cited as the best resource for quantifying the scope of services, but this data is quickly becoming outdated. When Kagawa et al.16 completed their analysis in 2012, an initial 2637 articles were identified through PubMed and Google Scholar, but only 3 had quantitative analysis of health systems, which shows the dearth of information on the impact of faith-based healthcare services. Other articles work to quantify the scope of healthcare services provided by FBOs,6-7,17-19 but this is usually done one country at a time. These articles are not consistent and do not all delineate between the type of service provided, if it is rural or urban, what each service location offers, how each location is organized, nor how to engage with these services. Some articles report the number of hospital beds, while others report on the number of facilities.
Many authors, policy makers, and FBOs want to cite a proportion of health services provided by FBOs, e.g., 20-70%, but that becomes difficult to interpret, especially as it varies widely from urban to rural areas. For example, in sub-Saharan Africa this proportion can be much higher in more rural areas, where the only hospital or clinic nearby is run by an FBO.10 Furthermore, because each faith-based organization has its own areas of emphasis or population focus, it can be difficult to compare services across FBOs. This lack of understanding was further brought to light at the start of the COVID-19 pandemic when health systems implemented fragmented responses.4-5,20-21 Finally, the number of faith-based healthcare facilities is dynamic, as facilities are closed and opened on a daily basis around the world.
Understanding the limitations and gaps of faith-based healthcare services allows us to address them and ultimately strengthen health systems — health systems flourish when all of their components are known and recognized for the important part they play. FBOs serve a significant proportion of the population in many countries and should have a seat at the table for health system governance and decision making, but in order to advocate for that seat, we have to clearly show the impact FBOs make.
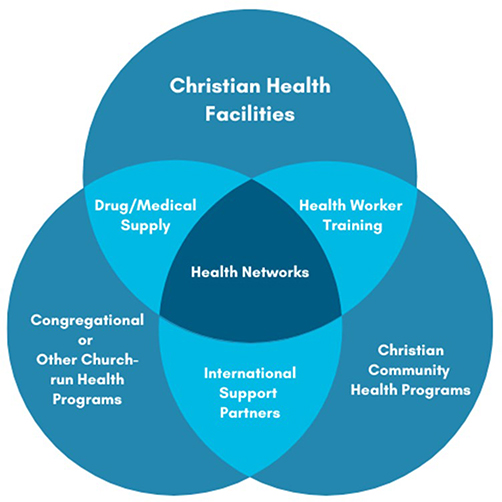
In response to this information gap, the Christian Health Asset Mapping Consortium (CHAMC) was launched in January 2022 by six founding organizations: Africa Christian Health Associations Platform (ACHAP), Catholic Health Association International Outreach (CHAIO), Christian Connections for International Health (CCIH), International Christian Medical and Dental Association (ICMDA), the Dalton Foundation, and the World Council of Churches (WCC). The Consortium hopes to create a better understanding of the nature, scope, and location of Christian health assets in LMICs at a summary level. The goal of the Consortium is to promote resources, learning, and partnerships in Christian health services in LMICs. By quantifying the healthcare services, CHAMC hopes to better the understanding of where and how Christian health assets operate within their diverse and dynamic contexts and systems. One feature that makes this initiative unique is CHAMC’s emphasis on registering all types of health assets in the Christian health landscape, not just facilities and hospitals. The following graphic demonstrates visually the Christian health assets landscape.
Christian Health Assets Landscape2
CHAMC set three initial objectives at its launch. First, it will create a metadata “registry” (or “database of databases”). Organizations and individuals can access this platform to better understand the known data sets that are already present, where the data comes from, how it is maintained, if it is accessible to the public, and the types of entities in a database. This database will be summary, protected, and will not identify individuals or facility contacts to protect their privacy. Second, it will support and inform stakeholders and policy by sharing information about Christian health services, including summary reports and referrals to specific data owners. Third, CHAMC will assess current available resources on Christian health assets and work to improve how these resources can be accessed and used to inform stakeholders.
To illustrate how this will work, CHAMC published a data brief in May 2023 to describe the scale of 22 Christian Health Associations (CHAs) in 17 countries in Sub-Saharan Africa. The study found 8,355 health assets ranging from national-level hospitals to community-level programs, training programs, and medical supply organizations.22 While this is a great starting point, we know that many health assets were missed. Data on additional assets and more countries are needed.
CHAMC receives a lot of questions about privacy of data. Some information we anticipate will be publicly available (e.g., a list of health training institutions in a country drawn from website data), while others will be managed as part of the work of local networks (such as health facilities or community programs). When the registry has a local dataset, CHAMC will list the dataset and who to contact for information about its constituents. They are best positioned to share further information.
A comprehensive data and mapping strategy is needed to accurately reflect the breadth and complexity of Christian health assets. If you or your organization are interested in engaging with the CHAMC, please reach out to mapping.consortium@ccih.org.