ORIGINAL ARTICLE
The prevalence and associated factors for anaemia in school children in Bengaluru, Karnataka, India: a cross-sectional study
Safder Husaina, Arish Mohammad Khan Sherwanib
a MD Unani in Tahaffuzi wa Samaji Tib [Community Medicine (Unani)], National Institute of Unani Medicine (an autonomous organisation under Ministry of AYUSH), affiliated with Rajiv Gandhi University of Health and Science. Bengaluru, India.
b Professor and HOD, Tahaffuzi wa Samaji Tib [Community Medicine (Unani)], NIUM (Rajiv Gandhi University of Health and Science), Bengaluru, India.
Abstract
Background and Objective: Anaemia is a common clinical condition that affects the majority of school aged children. Reduced resistance to disease, increased susceptibility to infection, impaired physical development, and poor school performance are all consequences of anaemia in this group. The present study was designed with the objective of estimating the prevalence of anaemia among school children in Bengaluru. This included identifying the associated factors or causes and consequences of anaemia.
Methods: A school based cross-sectional study was conducted among children in schools from 3rd to 8th standard in Bengaluru Urban North Division Karnataka State, India, over a period of one year. 250 children were selected using convenience sampling.
Results: The overall prevalence of anaemia among school going children was found to be 21.2%. Prevalence of anaemia was significant among variables like socioeconomic status, dietary habits, increased heart rate, breathlessness, lack of energy, dizziness, irregular menstrual cycles, jaundice, blood loss during menstruation, menstrual cycle pattern, pallor signs of palpebral conjunctiva, mucous membrane, and skin, splenomegaly and hepatomegaly, consumption of chicken, fish, citrus fruit, milk, Mizāj ‘Ām (overall mizaj of body, specifically choleric) duration of menstrual flow, headache, poor wound healing, and chronic disease.
Conclusion: The overall prevalence of anaemia in our study of school children in Bengaluru (21.2%) was lower than the prevalence in the data recently shown by NFHS-5. Prevalence of anaemia was highly significant among variables like low socioeconomic status, dietary deficiencies, blood loss, and chronic infections. There were also highly significant correlations with several clinical findings.
Key words: anaemia, prevalence, school children, public health, school health
Introduction
Anaemia is a condition in which the concentration of haemoglobin (Hb) in the blood is lower than the diagnostic reference range.1 In children, Hb reference ranges differ depending on the child’s age and the laboratory that is used in diagnosing the patient.2
Table 1. Normal cut–off values for diagnosing Anemia according to The WHO expert groups.3
| Age Group and Gender |
Normal Hb g/dl |
| Adult males |
13 |
| Adult females, non-pregnant |
12 |
| Adult females, pregnant |
11 |
| Children,6 months to 6 years |
11 |
| Children, 6 to 14 years |
12 |
Anaemia is still common in India, and its prevalence has increased across all age groups by 2–9% among infants, pregnant and non-pregnant women, and men, according to data from the National Family Health Survey 5 (NFHS-5) released on November 24, 2021. Karnataka is one of the worst-performing states, with a significant increase in occurrences of anaemia, having increased from 60.9% (NFHS-4) to 65.5% (NFHS-5).4 Anaemia has a multiple and complex aetiology and several factors influence anaemia in a population. Nutritional anaemia and non-nutritional anaemia in children are two categories based on the causes.5 The term “nutritional anaemia” covers all pathological conditions in which the blood haemoglobin concentration falls to a low level due to a deficiency in one or more nutrients. It is the most prevalent form of anaemia in the country. Iron deficiency is considered the most common nutritional deficiency, though other deficiencies can also cause anaemia, including deficiencies of vitamins A, B12, B6, C, D, and E, folate, riboflavin, copper, and zinc. Among these, vitamins A, B6, and B12, folic acid, and riboflavin are required for the normal production of RBCs, while vitamins C and E may protect RBCs through their antioxidant activity. Copper and zinc are trace elements found in the structures of enzymes involved in iron metabolism (e.g., copper and ceruloplasmin).6
Anaemia in children can have a variety of non-nutritional causes such as an increased iron requirement during adolescence, hookworm infestation, infections such as malaria or HIV, hemoglobinopathies like thalassemia, and loss of blood in the case of heavy menstrual bleeding.7
Some schools in India participate in regular deworming and iron and folic acid supplementation by the school authorities since 2003, as well as mid-day meal programmes including in the selected government schools included in this study.
Methods
The study was conducted in the Department of Tahaffuzi Wa Samaji Tib (Community Medicine/ Preventive and Social Medicine), National Institute of Unani Medicine, Bengaluru, India. Ethical approval was obtained from Institutional Ethical Committee (IEC) for Bio Medical researches, NIUM, Bengaluru prior to starting the study. This was a cross-sectional observational and epidemiological study conducted on school children in Bengaluru over a period of one year. A total of 250 students were studied from two government schools in Bengaluru’s urban North Division.
Criteria for selection of students
Students were enrolled in the study after fulfilling following selection criteria.
Inclusion criteria
- School going children of age group of 8 to 14 years.
- Children in school grades 3–8.
Exclusion criteria
- Children below 8 and above 14 years-of-age.
- Children in school below 3rd grade and above 8th grade.
Study design
School based cross-sectional study.
Sample size was based on the prevalence of anaemia taken from a study by Suchitra & Shashikumar (2014), calculated to be 246 by using the formula N=Z2 P(1-P)/D2 where N= Sample Size, Z= Level of confidence, D= Margin of error, P= Prevalence). By assuming 95% confidence level (Z), margin of error (D) 0.05%, and prevalence (P) was based on a previous study conducted among govt. school children of Bengaluru which was 80%. The sample size was round figured to 250. 8
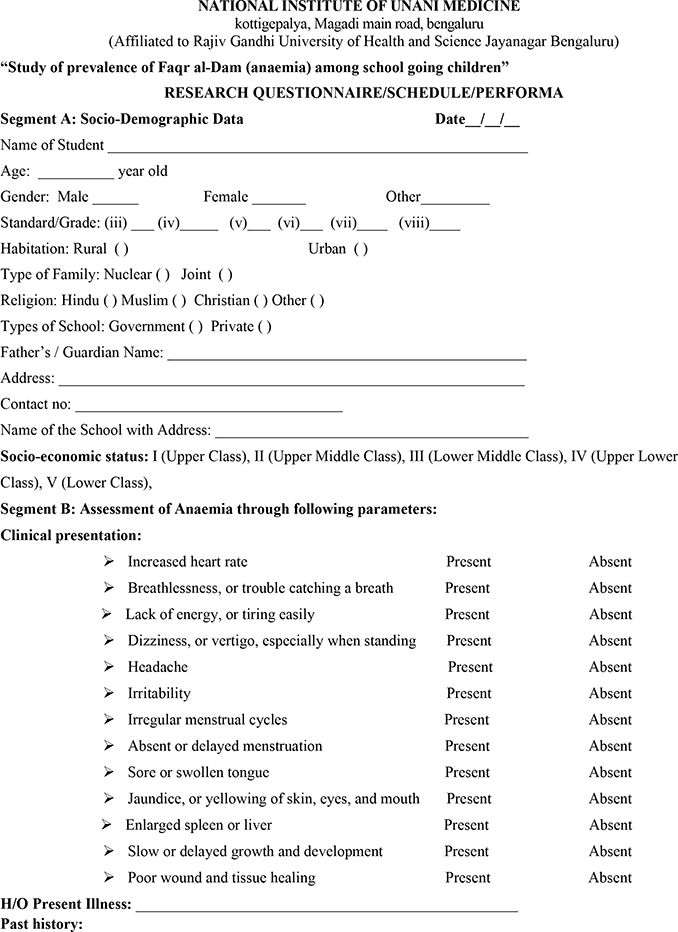
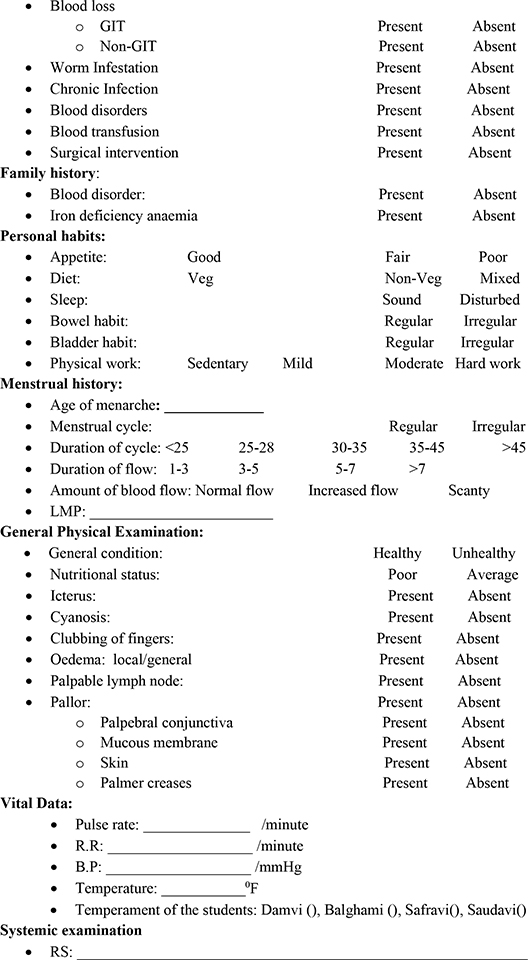
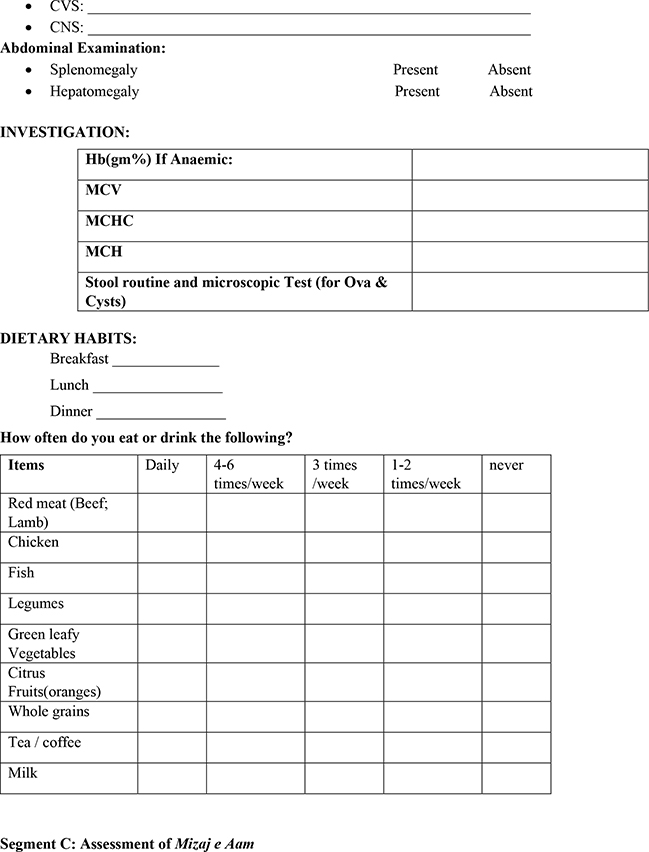
Tools for data collection
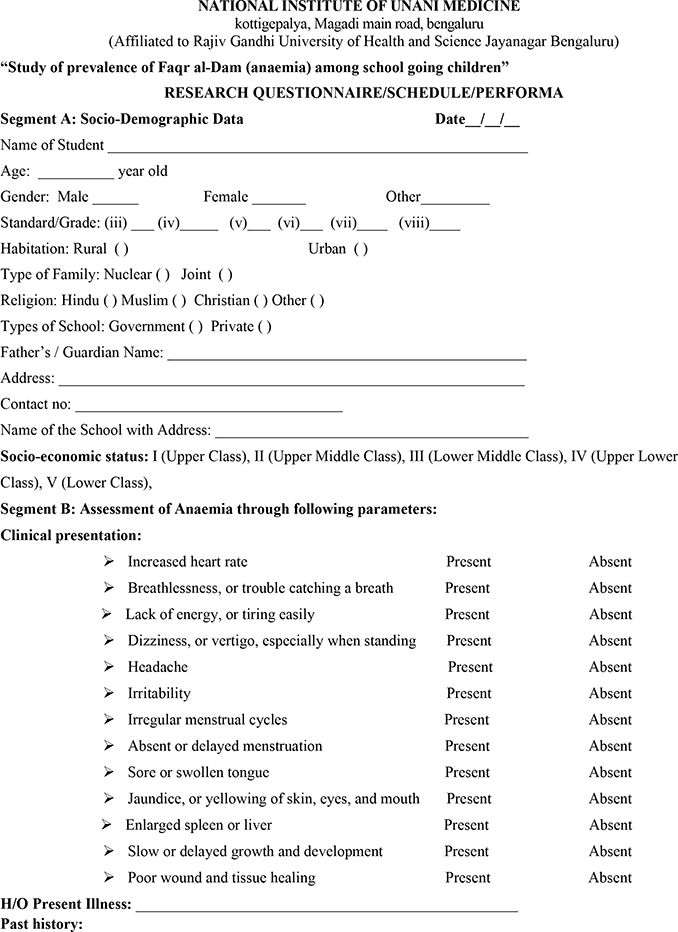
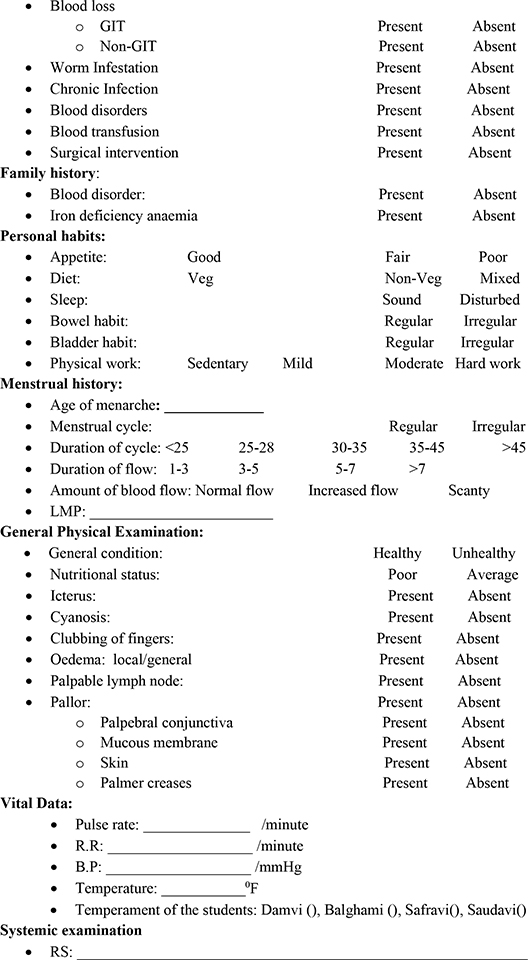
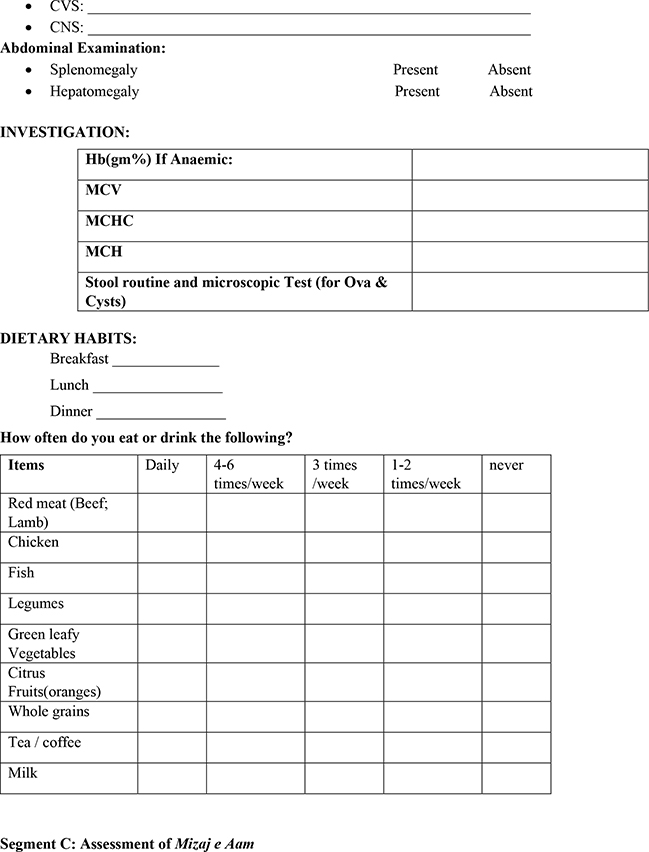
A questionnaire was designed to collect socio-demographic and personal data, including age, gender, socioeconomic status, and eating habits related to citrus fruit, meat, and green leafy vegetable consumption, systemic examination by the authors related to respiratory system, cardio-vascular system, central nervous system, abdominal examination related to splenomegaly and hepatomegaly, vital examination related to pulse rate, respiration rate, blood pressure, temperature, and Mizaj/temperament, clinical manifestation of anaemia and blood and stool examination related to Hb %, and if anaemic on screening the MCV, MCH, MCHC, and stool microscopic tests for ova and cysts. All this information was recorded in the questionnaire together with a written informed consent form in English or verbally translated into Kannada or Urdu.
Sampling technique
Sampling was done according to the permission granted by school staff and as per COVID-19 protocol. Permission was sought from the block education officers, principals and management of zones of both governments primary and middle schools for the assessments of anaemia and related health issues. After getting approval, we selected samples of school children belong to class 3rd to 8th standards as per the convenience sampling and feasibility of the schools’ timetable. We initiated the assessments of both schools until we reached the estimated sample size of 250 children. Criteria for selection of students was strictly followed, that is, inclusion and exclusion criteria.
Measurement of study variables
1. Socio-demographic variables: Students were queried about their name, sex, address, religion, types of families, and parents’ occupations.
2. Socio-economic status: Kuppuswamy modified classification of socio-economic status scale-2020 scale was used. Scores ranged as follows: 26–29 (Upper class I), 16–25 (Upper Middle class II), 11–15 (Lower Middle class III), 5–10 (Upper Lower class IV), and < 5 (Lower class V).
3. Diet: History of dietary habits regarding vegetarian and non-vegetarian diet was taken from the children. Questions were asked regarding skipping of meals and frequency of some foods (red meat, chicken, fish, legumes, green leafy vegetables, citrus fruits, whole grains, tea/coffee, and milk).
4. Past history:
a) Chronic diseases: Anaemia caused by several chronic diseases such as rheumatoid arthritis, rheumatic fever, SLE, leukaemia, and ankylosing spondylitis.11
b) Worm infestation: Intestinal bleeding caused by adult worms with blood in the stool in proportion to the parasite load in the intestine. 1–2 eggs of Ascaris lumbricoides were seen in our study. 12
5. Menstrual history: The pattern of the cycle (regular or irregular), the duration of flow in days (1–3, 4–6, > 7 days), and the amount of blood flow (scanty, moderate, heavy) was estimated by the number of pads used during the periods. The usual amount of blood loss per period is 10 to 35 ml. Each soaked normal sized tampon or pad holds a teaspoon (5ml) of blood. It is considered normal to soak 1 to 7 normal-sized pads or tampons (sanitary products) in a whole period per day. The amount of flow was measured by the number of pads used per day: normal flow (5–7 pads/day), increased/heavy flow (> 7 pads/day), and scanty flow (<1 pad/day).13
6. Clinical Manifestations: The following signs and symptoms were evaluated among all the subjects.
a) Pallor: Presence on skin, mucous membrane, lower palpebral conjunctiva, tongue, palm, and nails.14
b) Splenomegaly: Examined by palpation in the left hypochondriac region. If the spleen was found to be enlarged or a splenic mass moved downwards on inspiration, splenomegaly was suggested.15
c) Hepatomegaly: Examined by palpation in the right hypochondriac region.15
d) Tachycardia: Defined as a resting heart rate in an adolescent higher than 90 beats per minute.16
e) Swollen tongue: Presence of hypertrophic changes in the tongue.17
f) Breathlessness/Dyspnoea: Defined as a respiratory rate of more than 40 per minute in children.15
g) Lack of energy: Defined as a feeling of being low, tired, lethargic, or fatigued.
h) Dizziness/vertigo: Described a range of sensations, such as fainting, unsteadiness, and weakness. Vertigo was the sensation of the spinning of oneself or one’s surroundings.18
i) Headache: A painful sensation in any part of the head, ranging from sharp to dull.
j) Jaundice: A yellow discoloration of tissues and body fluids, examined on upper palpebral conjunctiva.15
k) Absent or delayed menstruation: Girls who had not reached menarche. Menstruation was considered as delayed if it commenced after 35 days.
l) Irregular menstrual cycle: Irregularities in menstrual cycle, e.g., menorrhagia, metrorrhagia.
m) Blood loss: Acute and chronic blood loss occurring due to any trauma, gastrointestinal tract lesions, or gynaecological disturbances.17
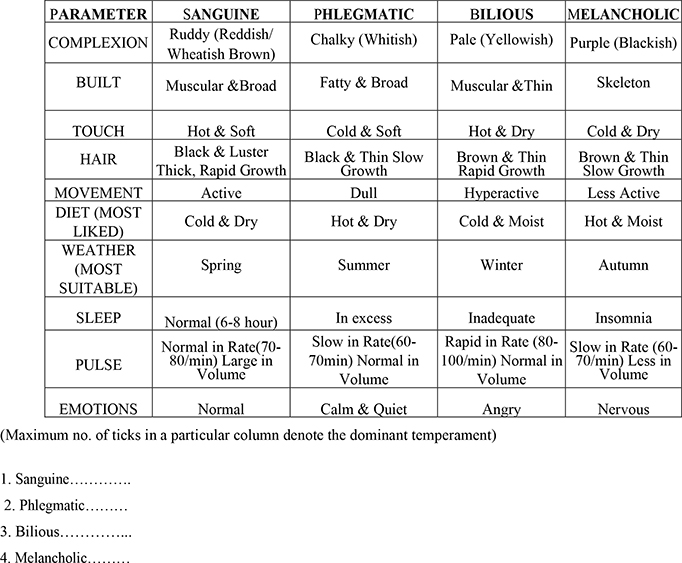
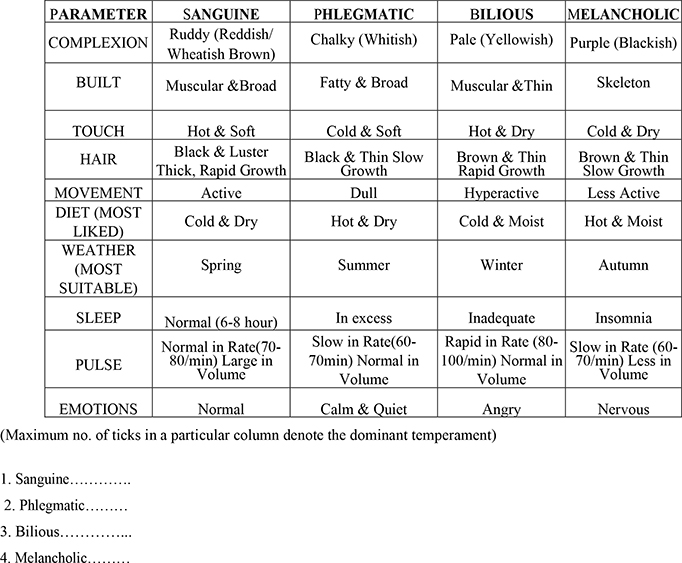
7. Mizaj (Temperament): This Unani traditional medicine approach based on the four conditions of Mizaj which were assessed by observation and self-assessment of 10 parameters including complexion, build, touch, hair, movement, diet, weather, sleep, pulse, emotion known as Ajnās ‘Ashara mentioned in Table 2 and scored by maximum number of ticks in a particular column of Mizaj denoted the dominant temperament or assessed Mizaj. Table 2 shows a list of assessment of Mizaj (temperament) parameters.
Table 2. List of Mizaj parameters
| PARAMETER |
SANGUINE |
PHLEGMATIC |
BILIOUS |
MELANCHOLIC |
| COMPLEXION |
Ruddy (Reddish/Wheatish Brown) |
Chalky (Whitish) |
Pale (Yellowish) |
Purple (Blackish) |
| BUILD |
Muscular &Broad |
Fatty & Broad |
Muscular &Thin |
Skeleton |
| TOUCH |
Hot & Soft |
Cold & Soft |
Hot & Dry |
Cold & Dry |
| HAIR |
Black & Luster Thick, Rapid Growth |
Black & Thin Slow Growth |
Brown & Thin Rapid Growth |
Brown & Thin Slow Growth |
| MOVEMENT |
Active |
Dull |
Hyperactive |
Less Active |
| DIET (MOST LIKED) |
Cold & Dry |
Hot & Dry |
Cold & Moist |
Hot & Moist |
| WEATHER (MOST SUITABLE) |
Spring |
Summer |
Winter |
Autumn |
| SLEEP |
Normal (6-8 hour) |
In excess |
Inadequate |
Insomnia |
| PULSE |
Normal in Rate(70-80/min)
Large in Volume |
Slow in Rate(60-70min)
Normal in Volume |
Rapid in Rate (80-100/min)
Normal in Volume |
Slow in Rate (60-70/min)
Less in Volume |
| EMOTIONS |
Normal |
Calm & Quiet |
Angry |
Nervous |
Method of collection of blood
After the questionnaire and physical exam were completed and recorded, blood was collected from children and tested for anaemia using the HemoCue (Hb 301) analyser within 10–20 sec at the school. Participants were classified as having mild (10-11.9 g/dl), moderate (7-9.9 g/dl), and severe (≤7.0 g/dl) anaemia based on WHO grading of anaemia.7 Following the blood collection, experienced nurses and lab personnel collected the samples and tested children, adolescent girls and boys. Samples were collected into microcuvettes and the filled cuvettes for the assessment of Hb%; on the spot collected blood samples were analysed by using a HemoCue (HB 301) analyser only. The Hb value was immediately displayed on the screen of the analyser and was recorded in proforma.9

Figure 1: HemoCue Hb 301
Note: A drop of whole blood was introduced into a plastic cuvette by capillary action. The cuvette was placed in the machine, which produces a direct read-out of haemoglobin to one decimal place. The procedure is depicted in the figure 1 HemoCue Hb 301.10
Statistical Methods
Each completed questionnaire was manually checked for completeness and consistency before it was tabulated in Microsoft Excel 2019. SPSS version 16.0, Vassar Stat, and SISA statistical software were used for the analysis of the data. Results of categorical measurements are presented in frequencies (numbers) and percentages. Significance was assessed at a .05% level. The Chi-Square/Fisher’s exact test was used to find the significance of study parameters on a categorical scale between two or more groups. Microsoft Word and Excel were used to generate tables and graphs.19
Ethics and CTRI procedure
The study was started following approval of the study protocol by the Institutional Ethical Committee, NIUM, Bengaluru, vide IEC No: NIUM/IEC/2019-20/036/TST/07 and Registration No: 07_U006_105670. The study was entitled “Study of Prevalence of Faqr Al-Dam (Anaemia) Among School Going Children.” It has been successfully registered in the Clinical Trials Registry-India (ICMR-NIMS) before the study. The Trial Acknowledgement Number is REF/2021/01/040240.
Results
Table 3 shows the prevalence of anaemia to be 21.2%. Mild anaemia accounted for 16.8%, moderate anaemia accounted for 4%, and severe anaemia accounted for just 0.4%.
Table 3. Prevalence of anaemia among subjects
| Grade of Anaemia |
No. of students |
% |
| Children without anaemia (Hb ≥12 gm/dL) |
197 |
78.8 |
| Children with anaemia (Hb ≤12 gm/dL) |
|
|
| Mild Anaemia (10-11.9 g/dl) |
42 |
16.8 |
| Moderate Anaemia (7-9.9 g/dl) |
10 |
4 |
| Severe Anaemia (≤7.0 g/dl) |
1 |
0.4 |
| Total |
250 |
100 |
Table 4 shows that the majority of the 53 anaemic children studied had hypochromic and normocytic (normal cell) anaemia 52.8%, hypochromic and microcytic anaemia 45.3%, and hypochromic and macrocytic (megaloblastic) anaemia only 1.9%.
Table 4. Distribution of Anaemia according to cell morphology
| Cell morphology on peripheral smear exam |
No of Anaemic Children |
% |
| Hypochromic and Normocytic |
28 |
52.8 |
| Hypochromic and Microcytic |
24 |
45.3 |
| Hypochromic and Macrocytic |
1 |
1.9 |
| Total |
53 |
100 |
Table 5 shows the list of different variables are used in the study and also mentioned in the questionnaire.
Table 5. List of Different Variables
| Variables |
Anaemic (n=53) |
Non-Anaemic (n=197) |
Total (n=250) |
P. value |
| Kuppuswamy socio economic scale-2020 |
| Upper Middle |
2 (12.5%) |
14 (87.5%) |
16 (100%) |
<.0001** |
| Lower middle |
8 (11.9%) |
59 (88.1%) |
67 (100%) |
|
| Upper lower |
27 (18.8%) |
117 (81.2%) |
144 (100%) |
|
| lower class |
16 (69.6%) |
7 (30.4%) |
23 (100%) |
|
| Dietary habits |
| Vegetarian |
37 (44%) |
47 (56%) |
84 (100%) |
<.0001** |
| Mixed |
16 (9.6%) |
150 (90.4%) |
166 (100%) |
|
| Clinical presentation |
| Increased heart rate |
| Present |
12 (80%) |
3 (20%) |
15 (100%) |
<.0001** |
| Absent |
41 (17.4%) |
194 (82.6%) |
235 (100%) |
|
| Breathlessness, or trouble catching a breath |
| Present |
17 (94.4%) |
1 (5.6%) |
18 (100%) |
<.0001** |
| Absent |
36 (15.5%) |
196 (84.5%) |
232 (100%) |
|
| Lack of energy, or tiring easily |
| Present |
49 (62.8%) |
29 (37.2%) |
78 (100%) |
<.0001** |
| Absent |
4 (2.3%) |
168 (97.7%) |
172 (100%) |
|
| Dizziness, or vertigo, especially when standing |
| Present |
33 (78.6%) |
9 (21.4%) |
42 (100%) |
<.0001** |
| Absent |
20 (9.6%) |
188 (90.4%) |
208 (100%) |
|
| Headache |
| Present |
25 (31.2%) |
55 (68.8%) |
80 (100%) |
0.0077** |
| Absent |
28 (16.5%) |
142 (83.5%) |
170 (100%) |
|
| Absent or delayed Menstruation (in total Female students, N=131) |
| Present |
2 (50%) |
2 (50%) |
4 (100%) |
0.237 |
| Absent |
29 (22.8%) |
98 (77.2%) |
127 (100%) |
|
| Irregular Menstrual cycles (in Total Female students, N=131) |
| Present |
12 (75%) |
4 (25%) |
16 (100%) |
<.0001** |
| Absent |
19 (16.5%) |
96 (83.5%) |
115 (100%) |
|
| Sore or swollen tongue |
| Present |
32 (100%) |
0 (0%) |
32 (100%) |
<.0001** |
| Absent |
21 (9.6%) |
197 (90.4%) |
218 (100%) |
|
| Jaundice, or yellowing of skin, eyes, and mouth |
| Present |
48 (78.7%) |
13 (21.3%) |
61 (100%) |
<.0001** |
| Absent |
5 (2.6%) |
184 (97.4%) |
189 (100%) |
|
| Slow or delayed growth and development |
| Present |
32 (82%) |
7 (18%) |
39 (100%) |
<.0001** |
| Absent |
21 (9.95%) |
190 (90.05%) |
211 (100%) |
|
| Poor wound and tissue healing |
| Present |
4 (80%) |
1 (20%) |
5 (100%) |
0.008** |
| Absent |
49 (20%) |
196 (80%) |
245 (100%) |
|
| Pallor Palpebral conjunctiva |
| Present |
48 (56.5%) |
37 (43.5%) |
85 (100%) |
<.0001** |
| Absent |
5 (3%) |
160 (97%) |
165 (100%) |
|
| Pallor Mucous membrane of mouth |
| Present |
30 (62.5%) |
18 (37.5) |
48 (100%) |
<.0001** |
| Absent |
23 (11.4%) |
179 (88.6%) |
202 (100%) |
|
| Pallor Skin |
| Present |
46 (85.2%) |
8 (14.8%) |
54 (100%) |
<.0001** |
| Absent |
7 (3.6%) |
189 (96.4%) |
196 (100%) |
|
| Splenomegaly |
| Present |
17 (100%) |
0 (0%) |
17 (100%) |
<.0001** |
| Absent |
36 (15.5%) |
197 (84.5%) |
233 (100%) |
|
| Hepatomegaly |
| Present |
20 (100%) |
0 (0%) |
20 (100%) |
<.0001** |
| Absent |
33 (14.3%) |
197 (85.7%) |
230 (100%) |
|
| Chronic Diseases |
| Blood loss |
| Present |
11 (100%) |
0 (0%) |
11 (100%) |
<.0001** |
| Absent |
42 (17.6%) |
197 (82.4%) |
239(100%) |
|
| Worm Infestation |
| Present |
2 (100%) |
0 (0%) |
2 (100%) |
0.044 |
| Absent |
51 (20.6%) |
197 (79.4%) |
248 (100%) |
|
| Chronic Infection |
| Present |
4 (80%) |
1 (20%) |
5 (100%) |
0.008** |
| Absent |
49 (20%) |
196 (80%) |
245 (100%) |
|
| Dietary Intake (Frequency times/ week) |
| Chicken |
| 1-2 T/W |
16 (10.4%) |
138 (89.6%) |
154 (100%) |
<.0001** |
| 3 T/W |
1 (6.3%) |
15 (93.7%) |
16 (100%) |
|
| Never |
36 (45%) |
44 (55%) |
80 (100%) |
|
| Fish |
| 1-2 T/W |
5 (4%) |
119 (96%) |
124 (100%) |
<.0001** |
| 3 T/W |
0 (0%) |
2 (100%) |
2 (100%) |
|
| Daily |
0 (0%) |
1 (100%) |
1 (100%) |
|
| Never |
48 (39%) |
75 (61%) |
123 (100%) |
|
| Green leafy vegetables |
| 1-2 T/W |
0 (0%) |
13 (100%) |
13 (100%) |
< 0.05 |
| 3 T/W |
15 (25.4%) |
44 (74.6%) |
59 (100%) |
|
| 4-6 T/W |
26 (26%) |
74 (74%) |
100 (100%) |
|
| Daily |
12 (15.4%) |
66 (84.6%) |
78 (100%) |
|
| Citrus Fruits (Oranges) |
| 1-2 T/W |
27 (18.9%) |
116 (81.1%) |
143 (100%) |
<.0001** |
| 3 T/W |
2 (15.4%) |
11 (84.6%) |
13 (100%) |
|
| 4-6 T/W |
2 (16.7%) |
10 (83.3%) |
12 (100%) |
|
| Daily |
7 (10.9%) |
57 (89.1%) |
64 (100%) |
|
| Never |
15 (83.3%) |
3 (16.7%) |
18 (100%) |
|
| Whole grains |
| 1-2 T/W |
2 (22.2%) |
7 (77.8%) |
9 (100%) |
0.427 |
| 3 T/W |
2 (28.6%) |
5 (71.4%) |
7 (100%) |
|
| 4-6 T/W |
13 (29.5%) |
34 (70.5%) |
47 (100%) |
|
| Daily |
36 (20.1%) |
143 (79.9%) |
179 (100%) |
|
| Never |
0 (0%) |
8 (100%) |
8 (100%) |
|
| Milk |
| 1-2 T/W |
17 (58.6%) |
12 (41.4%) |
29 (100%) |
<.0001** |
| 3 T/W |
4 (40%) |
6 (60%) |
10 (100%) |
|
| 4-6 T/W |
0 (0%) |
6 (100%) |
6 (100%) |
|
| Daily |
17 (10.1%) |
152 (89.9%) |
169 (100%) |
|
| Never |
15 (41.7%) |
21 (58.3%) |
36 (100%) |
|
| Mizaj e Aam |
| Damvi (Sanguinic) |
3 (2.0%) |
145 (98%) |
148 (100%) |
<.0001** |
| Balghami (Phlegmatic) |
1 (2.4%) |
41 (97.6%) |
42 (100%) |
|
| Safravi (Choleric) |
48 (87.3%) |
7 (12.7%) |
55 (100%) |
|
| Saudavi (Melencholic) |
1 (20%) |
4 (80%) |
5 (100%) |
|
| Menstrual History (Female students) |
| Menstrual Cycle |
| Regular |
17 (19.5%) |
70 (80.5%) |
87 (100%) |
<.0001** |
| Absent |
4 (12.9%) |
27 (87.1%) |
31 (100%) |
|
| Irregular |
10 (76.9%) |
3 (23.1%) |
13 (100%) |
|
| Total |
31 (23.7%) |
100 (76.3) |
131 (100%) |
|
| Duration of Flow |
| 1 to 3 days |
8 (20.5%) |
31 (79.5%) |
39 (100%) |
0.006** |
| 3 to 5 days |
9 (20.5%) |
35 (79.5%) |
44 (100%) |
|
| 5 to 7 days |
10 (58.8%) |
7 (41.2%) |
17 (100%) |
|
| Absent |
4 (12.9%) |
27 (87.1%) |
31 (100%) |
|
| Total |
31 (23.7%) |
100 (76.3) |
131 (100%) |
|
| Amount of blood flow |
| Normal Flow |
17 (19.5%) |
70 (80.5%) |
87 (100%) |
<.0001** |
| Increased |
10 (76.9%) |
3 (23.1%) |
13 (100%) |
|
| Absent |
4 (12.9%) |
27 (87.1%) |
31 (100%) |
|
| Total |
31 (23.7%) |
100 (76.3) |
131 (100%) |
|
Discussion
In the present study, we have used various established variables of anaemia and found the level of significance of the association among them. These variables have been described separately in ancient Unani literature and modern scientific research as well, either as causes or consequences of childhood anaemia. We have observed the association with anaemia in variables like socioeconomic status, diet, clinical presentation, chronic infection, signs of pallor, dietary intake, Mizaj e Aam, and menstrual history.
The total prevalence of anaemia was 21.2% of children in this study. The prevalence according to severity was as follows: the majority (79.2%) had mild grade anaemia, moderate anaemia prevalence was 18.9%, and severe anaemia was only 1.9%. The anaemia prevalence in our study was similar to that of Kumar T et al;20 the WHO research studied children worldwide, where the prevalence was 39.8%.21 The reason for our lower prevalence could be regular deworming and iron and folic acid supplementation by the school authorities in Bangalore since 2003.20,21
The present study revealed that the prevalence of anaemia varies among different socio-economic classes with the correlation being significant (P<.0001). Anaemia was more prevalent among V (lower class). This may be due to low literacy status and poor nutrition as found in a study by Kavthekar S et al. 22 Anaemia and dietary habits were significantly correlated (P<.0001) and the majority were vegetarians. This was due to poor bioavailability of dietary iron coupled with a low intake of haem iron derived from animal food and a low intake of green leafy vegetables and dairy products. Major components of the diet in developing countries like India are cereals and roots, which are not favourable for iron absorption as compared to meat and fish. The frequency and amount of consumption of non-vegetarian food among the studied population was quite low as a greater number of lower socioeconomic status children were included in our study, consistent with a study by Ayushi Agrawal et al.23
The present study observed the following clinical presentations of anaemia which included swollen tongue, enlarged spleen or liver, increased heart rate, breathlessness, vertigo, irregular menstrual cycle, and delayed growth (P<.0001). Headache (P=0.007) and poor wound healing (P=0.008) were significantly associated with anaemia. This reflected the fact that anaemia is often asymptomatic, and has non-specific signs and symptoms unless the anaemia is severe.
On statistical analysis, occurrence of anaemia was found to be significant for blood loss (P<.0001), worm infestation (P=0.044), and chronic infections (P=0.008), respectively. Tiwary et al. observed in a similar study that hook worm associated anaemia in children was higher by 23.57%. This may be due to poor hygienic practices, poor educational background, poor sanitation, unsafe drinking water, use of contaminated food, and lack of health awareness.24
Statistical analysis revealed a significant relationship between anaemia and irregular menstrual cycles (P<.0001). Blood losses associated with menstruation are a common cause of iron deficiency. Typically, non-menstruating women lose about 1 mg of iron per day, while menstruating women lose an additional 10 mg of iron per day during menses. When combined with greater and heavier blood loss during menstruation, even a regular menstrual cycle can cause anaemia, as found in the present study. Statistical analysis revealed a significant relationship (P=0.006) with anaemia. Menstrual cycle pattern was also significantly associated (P<.0001) with anaemia because it represents greater blood loss on average during one menstrual cycle. Heavy menstrual bleeding is a common cause of iron deficiency and iron deficiency anaemia in women of reproductive age. 25
Statistical analysis revealed a significant relation between anaemia and pallor signs (P<.0001). Our study was closely related to the study of Keshav K et al., which also found a significant difference (P<0.001) between anaemia and a pallor signs.26
Our study showed that splenomegaly and hepatomegaly have a significant relationship with anaemia (P<.0001). There was no known research on the relationship between anaemia and hepatosplenomegaly. However, our findings are possibly due to red blood cell sequestration in the spleen that lowers the effective circulating mass of red blood cells.27 We found a significant relationship between anaemia and reduced chicken consumption (P<.0001). This significant relationship is consistent with the study conducted by Divyamol N et al., which showed that low consumption of chicken was associated with anemia.28 We also found low fish consumption to have a significant relationship to anaemia (P<.0001). Fish is a good source of iron because it is bioavailable.3 Anaemia was shown to be less present among those who consumed green leafy vegetables (P<0.05). These data support the importance of these foods in terms of nutrition. Green leaves are high in carotenes, calcium, iron, and vitamin C, with the exclusion of vitamin B12 (an iron absorption promoter).3 Anaemia and citrus fruit eating were found to have a statistically significant connection (P<.0001) across all consumption groups, with the highest number of affected subjects. The probable explanation for this finding may be that citrus is an excellent source of vitamin C. Most people can achieve 100% of the RDA for vitamin C by consuming moderate amounts of citrus fruit. Asians consume approximately 71 gm per capita per day. Vitamin C (ascorbic acid) is a water-soluble essential nutrient that acts as an antioxidant and is involved in iron metabolism as an iron absorption promoter.3 Increased occurrences of anaemia in those group may be due to some other factors like reduced B12 in leafy vegetable, socioeconomic reasons, etc. The prevalence of anaemia was found to have a statistically significant connection with reduced milk consumption (P<.0001). Our findings are similar with that of El Menchawy I et al. who found a significant effect (P=0.037) in Moroccan school children. The results showed that milk drinking reduced iron deficiency from 50.9% to 37.2% of dietary iron absorption.29 There was a significant correlation between anaemia and Mizaj according to statistical analysis (P<.0001). This significantly high occurrence of Choleric Mizaj among anaemic school going children was in accordance with the Unani concept, which states that Sanguinic Mizaj was related to the higher production of khilt Dum (Blood) in comparison to other Mizaj groups. This sequence of blood production decreases with Phlegmatic Mizaj as phlegm is considered as immature or unripped blood (kachcha khoon) that leads to formation of mature RBC or blood if there is no dietary deficiency. Choleric and Melancholic temperaments have more disintegration of blood or RBC to yellow bile (Bilirubin, Biliverdin) and black bile (people with benign lesion, moles or cancerous lesion), respectively.30,31
In Unani system of medicine all human beings have distinguished mizaj which is classified into four qualitative categories: 1. Damvi (sanguineous), 2. Safravi (bilious), 3. Balghami (phlegmatic), and 4. Saudavi (melancholic). This classification is based on four humoral theories in which every person has a holistic Mizaj as a whole and every organ of the body has also its unique Mizaj that varies from person to person. In the Unani System of Medicine, Mizaj (Temperament) acts as a basis for diagnosis and treatment. The evaluation and classification of temperaments is based on the intermixture of four akhlat (humours) in varying quantities in the blood, so blood plays a key role in the constitution of Mizaj. Domination of humours, such as blood, phlegm, bile, and black bile in the blood classifies people as sanguine, phlegmatic, choleric, or melancholic.32
According to the Unani physicians Ibn Sina, Ismail Jurjani, Ibn Hubal Baghdadi, and Hakim Azam Khan blood is considered to be the vital fluid of human body which is formed in the liver. Due to derangement of the liver functions and weakness of hepatic faculties, or sometimes due to associated disease, the resultant formation of blood in normal for nourishment there by leading to anaemia. 33,34 Razi (Razes, 841-926AD) and Abul Hasan Ahmad Bin Mohammad Tabri (10th century AD) have mentioned that sū mizāj kabid bārid wa rātāb (deranged cold and wet temperament of liver), leads to the development of features of iron deficiency anaemia, which they have described as Sū’al-Qinya.35 The word Sū’al-Qinya was coined by Ismail Jurjani (12th C AD). Sū means defect and Qinya means treasure, therefore anaemia might be considered a treasury defect.36
According to Unani medicine, various synonyms (20th century term: Faqr al-Dam, Century-old terms: Sū’al-Qinya, Qillat-i-dam, khoon-ki-Kami, khoon ki mohtaji (ghareebi,nadari) and Fas̄ad al-Dam.37) for anaemia were used.
Faqr al-Dam is a word in Arabic that means “blood shortage or loss.” The Arabic word “Sū ’al-Qinya” refers to a storage change or deficiency, which is linked to the iron or dietary deficiency anaemia. Some Unani physicians refer to Sū’al-Qinya as “Ḍu‘f al-jigar” (weakness of the liver due to impaired metabolism of liver), while others refer to it as “Sū’-i- Mizāj” (an imbalance of individual’s temperament). Others have called it “Ridhayat-e-dam” which refers to changes in blood quality or morphology (like hyper chromic, hypochromic, and size of cells), and concentration, odour, viscosity, temperature, and colour as well.38
Limitations of the study
1. The study used a school health survey when schools were opened for a limited period in Karnataka. The school management and principals were not fully cooperative to allow the investigators to conduct the study and to obtain blood and other investigations. So convenient sampling technique was used over a year’s time.
2. Anaemia diagnosis was based on Hb% and cell indices, and aetiologies were not further confirmed by serum ferritin or other tests due to lack of facilities and resources.
3. The study was conducted only in urban areas.
Conclusion
The overall prevalence of anaemia in our study of government school children in Bengaluru (21.2%) was lower than the prevalence in the data recently shown by NFHS-5.
Prevalence of anaemia was highly significant among variables like low socioeconomic status, dietary deficiencies (low consumption of chicken, fish, citrus fruit, and milk), heavy blood loss during menstruation, and irregular menstrual cycle patterns, and chronic infections. There were also highly significant correlations with clinical findings of increased heart rate, breathlessness, lack of energy, dizziness or vertigo, sore or swollen tongue, jaundice, enlarged spleen or liver, delayed growth, headache, poor wound healing, and pallor of palpebral conjunctiva, mucous membrane, and skin. Mizāj ‘Ām correlated significantly with the Safravi (Choleric) temperament.
Anaemia is still a major burden in children of India, even in areas with school-based interventions, so this suggests further longitudinal studies are needed to asses school-based or community interventions.
References
- Britannica, T. Editors of Encyclopaedia (2020, December 15). Haemoglobin [Internet]. Encyclopedia Britannica. Available from: https://www.britannica.com/science/haemoglobin
- Uppal N, Sharma A, Kukreja S. A study of prevalence of anemia in pediatric population in a tertiary care hospital in Amritsar. Int J Clin Biochem Res. 2019;6(3):396-400. https://doi.org/10.18231/j.ijcbr.2019.085
- Park K. Text Book of Preventive and Social Medicine. 25th Edition. Jabalpur: Banarsidas Bhanot Publisher; 2019:280,677-87. [680,681,684,685,687]
- Anonymous. National family health survey (NFHS-5)-State fact sheet Karnataka [Internet]. Mumbai: International Institute for Popular Ion Science, Ministry of health and family welfare; 2019-20. Available from http://rchiips.org/NFHS/NFHS-5_FCTS/NFHS 5%20State%20Factsheet%20Compendium_Phase-I.pdf
- Gupta A, Lal PR, Sharma LK, Prakash S. Understanding the determinants of anaemia amongst Indian adolescents. Int J Health Sci Res. 2021;11(4):213-35. https://doi.org/10.52403/ijhsr.20210428
- Chaparro CM, Suchdev PS. Anemia epidemiology, pathophysiology, and etiology in low-and middle-income countries. Annals New York Acad Sci. 2019 Aug;1450(1):15. https://doi.org/10.1111/nyas.14092
- Anonymous. Technical handbook on anemia in adolescents [Internet]. Available from https://www.nhm.gov.in/images/pdf/programmes/wifs/guidelines/technical_handbook_on_anemia.pdf
- Devi HS. Prevalence of anemia among Indian children of various age groups–a systematic review. J Advances Med Pharm Sci. 2019 Jun 17:1-6. https://doi.org/10.9734/jamps/2019/v20i430117
- Ramesh S, Kumar D, Bagavandas M. Prevalence of anemia among school going adolescent girls and boys (10-18 years) in South India-a community based cross sectional study. Annals Romanian Soc Cell Biol. 2021 Jun 5;25(6):7842-7. https://www.annalsofrscb.ro/index.php/journal/article/view/6975
- Bates I, McKew S, Sarkinfada F Anemia: a useful indicator of neglected disease burden and control. PLoS Med 2007;4(8): e231. https://doi.org/10.1371/journal.pmed.0040231
- Raftery AT, Lim EK, Ostor AJ. Churchill’s pocketbook of differential diagnosis e-book. Elsevier Health Sciences; 2014 Mar 18;26:423. https://www.google.co.in/books/edition/Churchill_s_Pocketbook_of_Differential_D/W_1sAwAAQBAJ?hl=en&gbpv=0
- Singh Y, Gupta A, Yadav R. Incidence of anemia among hookworm infection in tertiary care hospital. Galore Int J Health Sci Res. 2019;4(4):72-5.
- Prior JC. Very heavy menstrual flow [Internet]. Available from https://www.cemcor.ubc.ca/resources/very-heavy-menstrual-flow
- Peterson P, Cornacchia MF. Anemia: pathophysiology, clinical features, and laboratory evaluation. Lab Med. 1999 Jul 1;30(7):463-7.
- Mehta SP, Mehta NP, Joshi SR. PJ Mehta’s practical medicine. The National Book Depot; 2013. p. 19,20,22,23,65,67,125.
- Anonymous. Types of arrhythmia in children [Internet]. Available from https://www.heart.org/en/health-topics/arrhythmia/about-arrhythmia/types-of-arrhythmia-in-children
- Kumar V, Abbas A, Aster J. Robbins and Cotran, Pathologic basis of disease: South Asia edition. Vol.1. New Delhi: Elsevier India; 2014: p. 1-29,630,652,633.
- Anonymous. Dizziness [Internet]. Available from https://www.mayoclinic.org/diseases conditions/dizziness/symptoms causes/syc-20371787
- Rakesh PS, George LS, Joy TM, George S, Renjini BA, Beena KV. Anemia among school children in Ernakulam district, Kerala, India. Indian J Hemato Blo. 2019 Jan;35(1):114-8. https://doi.org/10.1007%2Fs12288-018-1001-6
- Kumar T, Solanki S, Vadhera M, Joshi N. Analysis of incidence of anemia among school going children. J Adv Med Dental Sci Res. 2021 Apr;9(4). https://doi.org/10.21276/jamdsr
- Mutthayya S, Thankachan P, Zimmermann MB, Andersson M, Eilander A, Misquith D, et al. Low anemia prevalence in school-aged children in Bangalore, South India: possible effect of school health initiatives. E J Clin Nutr. 2007 Jul;61(7):865-9. https://doi.org/10.1038/sj.ejcn.1602613
- Kavthekar S, Kulkarni D, Kurane A, Chougule A. Association of BMI, socioeconomic status and menarche age with anemia in rural school going adolescent girls. Int J Pediatr Res. 2016;3(7):486-92. https://doi.org/10.17511/ijpr. 2016.i07.04
- Agrawal A, Shetty A, Jacob GP, Kamath A. Anemia among adolescents in a coastal district of India. Natl J Community Med.2018;9(6):396-401. https://njcmindia.com/index.php/file/article/view/726
- Tiwary SK, Sharan S, Singh BK, Sinha SK, Kumar R. Prevalence of anemia in hookworm infestation in children of slum areas in and around Dhanbad. Int J Contemp Med Res. 2018 Sept;5(9):11-13. https://www.ijcmr.com/uploads/7/7/4/6/77464738/ijcmr_2153.pdf
- Wang W, Bourgeois T, Klima J, Berlan ED, Fischer AN, O’Brien SH. Iron deficiency and fatigue in adolescent females with heavy menstrual bleeding. Haemophilia. 2013 Mar;19(2):225-30. https://doi.org/10.1111/hae.12046
- Keshav K, Pathak SK, Kumar S, Kumar B. A case-control study to evaluate the precision of pallor in the diagnosis of anemia. European Journal of Molecular & Clinical Medicine (EJMCM).;7(10):2020.
- Mazigo HD, Lwambo NJ, Mkoji GM, Laurent LM, Kweka EJ, Waihenya R. Anemia and organomegaly associated with parasitic infections among schoolchildren in Sengerema District, North-Western Tanzania. Tanz J Health Res. 2010;12(2):121-8. https://doi.org/10.4314/thrb.v12i2.56399
- Divyamol N, Sajna MV. Prevalence of anemia among adolescent girls in a rural area of Central Kerala, South India. Int JCommun Med Public Health. 2022 Feb;9(2):698. https://dx.doi.org/10.18203/2394-6040.ijcmph20220226
- El Menchawy I, El Hamdouchi A, El Kari K, Saeid N, Zahrou FE, Benajiba N, et al. Efficacy of multiple micronutrients fortified milk consumption on iron nutritional status in Moroccan schoolchildren. J Nutri Metab. 2015 Jan 1;1-8. https://doi.org/10.1155/2015/690954
- Ibn Sīnā al-Shaykh al-Ra’īs Abū ‘Alī al-Ḥusayn ibn ‘Abdullāh. Al-Qānūn fi’l Ṭibb (Urdu Translation by Ghulām Ḥasnayn Kintūrī). Vol.1. New Delhi: Idāra Kitābus Shifā’; 2010: p. 28-30,33-34,137,884-85,892-93.
- Baghdādī Ibn Hubal. Kitāb al-Mukhtārāt fi’l Ṭibb (Urdu Translation by CCRUM). Part.I. New Delhi: CCRUM; 2005: p. 29.
- Hussain MI, Hussain A. Concept of temperament in Unani system of medicine: a review. The Pharma Innova J. 2019;8(9):07-11. https://www.thepharmajournal.com/archives/2019/vol8issue9/PartA/8-9-5-949.pdf
- Kantoori S.G.H H. Tariuma Qanoon vol 3rd part 2 (original author shaikh ali bin Abdullah ibn-e-sina) munshi Nawal Kishore Kanpur, 1303; p.47-53.
- Kabeeruddin HM. Tariuma Kabeer Sharah-e-Asbab (vol 2nd). (Original author, Nafis Bin Euz Kirmani) Hikmat book depot. Hyderabad, 1950; p.669-688.
- Verma, RS, Parveen S, Khan AL. The efficacy and safety of an Unani Pharma- copoeial Drug Sharbat-E- Faulad in cases of anemia. Hippocratic J Unani Med.2013, 8(3): 11-21. https://www.unanijournal.com/articles/160/5-1-1-140.pdf
- Jurjani I, Zakhira Khwarzam Shahi.Vol.6. New Delhi: Idara Kitabus Shifa;2010. p.29-30,105,385,426,652.
- Samarqandi N. molejaat sharah asbab (translation by Kabeeruddin H). Vol. 1. New Delhi: Idara Kitabus Shifa; 2009; p.560-3.
- Azam HM. Akseer-e-Azam, Urdu translation by Hkm. Kabiruddin. New Delhi; Idara Kitab-us-Shifa, 2011; p.519-21
Peer Reviewed: Submitted 7 May 2023, revised 4 Jul 2023, accepted 19 Jul 2023, published Oct 2023
Competing Interests: None declared.
Correspondence: Safder Husain, Bengaluru, India.
shjafry65@gmail.comAcknowledgements: Prof. Abdul Wadud Director NIUM Bengaluru, provided facilities for cross sectional survey in their institute NIUM Bengaluru under the Central Govt. of India. The author is thankful for their contribution.
Conflict of interests: None declared.
Cite this article as: Husain S, Sherwani AMK. The prevalence and associated factors for anaemia in school children in Bengaluru, Karnataka, India: a cross-sectional study. Christ J Glob Health October 2023; 10(2):22-36.
https://doi.org/10.15566/cjgh.v10i2.773© Authors. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are properly cited. To view a copy of the license, visit
http://creativecommons.org/licenses/by/4.0/
Appendix